Not everything was illuminated in health IT survey
Posting of 2015 Health Information Technology survey findings offer a lot to digest
PROVIDENCE – There is a lot to unpack in the recent online posting of the results of the 2015 Health Information Technology, or HIT Survey, conducted by the R.I. Department of Health in the spring of 2015.
First, the biggest question is why had there been such a long delay in releasing the results, given that the final tabulations were available on Sept. 22, 2015, according to the dates on the document.
Second, although some parts of the HIT survey made it into the first-ever comprehensive statewide health inventory released on Nov. 17, 2015, some parts did not – in particular, the updating of the 2015 results on the use of CurrentCare. [See link to ConvergenceRI story below.]
A more detailed analysis of the Rhode Island’s health IT infrastructure had been promised to be released in early 2016, one that incorporated all the findings of the 2015 survey, according to health department officials. That report, associated with the statewide health inventory, is still being written, according to health department spokesman Joseph Wendelken.
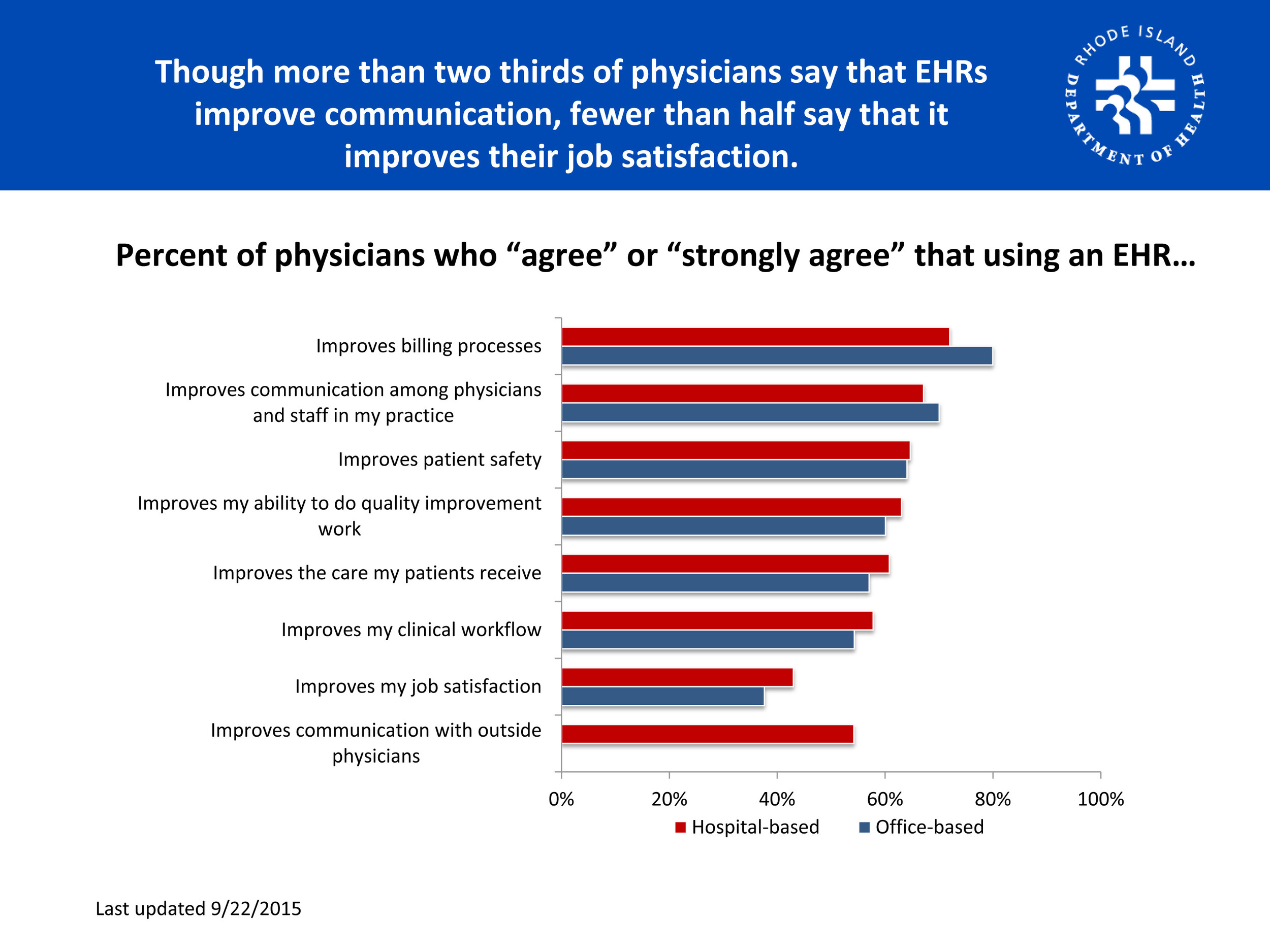
Third, the survey documents that more than two-thirds of Rhode Island physicians “agree strongly” or “agree” that using electronic health records improves billing processes and improve communications, but fewer than half say that it improves their job satisfaction.
The lack of improvement in job satisfaction belies a more telling observation. “I was impressed by [the fact] many primary care physicians do not seem to be happy with their practices and that the HIT movement is not improving their satisfaction,” said Dr. Peter Simon, a pediatrician and epidemiologist who reviewed the document at ConvergenceRI’s request.
Further, Simon continued, “I think there had better be more attention paid to physician practice satisfaction. Or else forget about the primary care physician workforce and expand the role of nurses and other non-physician providers.”
Fourth, while there are some questions and analysis of the findings related to population health management analytics within the framework of the survey, thare appear to be some significant gaps, in particular, the larger context of the move from fee-for-service to accountable care entities, bring driven by changes in Medicaid and Medicare reimbursements.
This is a particularly critical aspect of health IT implementation moving forward, given the rapidity with which the R.I. Executive Office of Health and Human Services is launching five accountable entities pilots for the managed Medicaid population, in order to meet the deadlines mandated by the Reinventing Medicaid statute.
To be successful in moving toward a payment system that rewards value over volume in a continuum of care for the patient, it requires the capability to measure the patient’s health outcomes across a number of platforms and metrics. To accomplish this, it requires the interoperability to connect and share information – provider to provider – across health IT systems.
It may seem like getting into the weeds here, but the interoperability of sharing data in real time can be done through what’s known as Consolidated Clinical Document Architecture, or CCDA. Practices can import and send patients’ critical data in real time, through what’s called a direct connection that employs a Health Information Service Provider, or HISP.
In Rhode Island, the HIT survey found that less than one-sixth of physician practices – 12.6 percent hospital-based practices and 16.5 percent of office-based practices – had a direct address, i.e., a specific electronic address for secure messaging using a HISP. Worse, the majority – 61.9 percent of hospital practices and 55.7 percent of office-based practices – said they didn’t know.
That is a worrisome statistic, according to some health care industry observers.
CurrentCare
The 2015 HIT survey found that most hospital and office-based physicians were not signed up to view or receive CurrentCare data, mirroring the results of the 2014. In 2015, the survey found that 74 percent of Rhode Island physicians said that they were not signed up to receive or view data from CurrentCare, another 12.9 percent were signed up but not using it, and only 13.1 percent said that they were using it for some or all of their patients.
Further, office-based physicians were more likely than hospital-based practices to be familiar with CurrentCare services, such as the CurrentCare Viewer, the CurrentCare Inquiry, Hospital Alerts or EHR Integration. But, in terms of penetration of the market, the levels of familiarity were at the lower end of the scale: only the CurrentCare Viewer reached a segment larger than 25 percent familiarity among all physicians [28.8 percent].
In October of 2015, in an interview with ConvergenceRI, Laura Adams, the president and CEO of the Rhode Island Quality Institute, which directs CurrentCare, addressed the apparent lack of buy-in that the numbers from the survey showed. [See link to ConvergenceRI story below.]
Adams acknowledged that from what she had seen in the preliminary numbers from the 2015 HIT survey, there had not been a whole lot of change in the numbers from the 2014 survey.
“This was a survey conducted of the whole population of physicians,” Adams explained. What we’re finding is that the usage of CurrentCare is accelerating most rapidly around nurse care managers, and among other team members that are responsible for quality improvement and quality reporting.”
Further, Adams said: “We also realized that when physicians say that they don’t use CurrentCare, it could be very well that their nurse care manager [were using] it every day.”
And, she added: “The survey doesn’t count alerts, it just counts one component of CurrentCare, not another component of CurrentCare.
Our concern with that survey now is that it is [calculating] one set of metrics, around how CurrentCare is used, and there are about five or six different ways that you can use it now.
Finally, Adams said: “We still measure logins, as in how many people log into CurrentCare. What we realized was that the number was problematic, because you could log in and look at 30 charts, and it would be counted as just one log in.”
Patient-driven health IT
In the Jan. 21 edition of the New England Journal of Medicine, Dr. Kenneth D. Mandl and Dr. Isaac S. Kohane offered a provocative view of the current health IT conundrum, asking whether it was: “Time for a Patient-Driven Health Information Economy?
They wrote: “Nearly two thirds of Americans own smart phones, with online access, apps, and both local and cloud storage of data. As health care reimbursement shifts toward risk-based contracting, providers seek to understand the totality of patients’ experience, which requires aggregating data across care silos.”
They continued: “As the clinical research infrastructure accommodates pragmatic studies and incorporates patient-centered outcomes in therapeutics development, patients are increasingly asked to report on adverse events and end points and donate health data to trials.”
They added: “Fortunately, the belief that it’s dangerous to allow patients access to health data is slowly dissolving, with the advent of programs such as Beth Israel Deaconess Medical Center’s Open Notes, in which doctors and patients jointly read and create chart entries.”
Mandl and Kohane reported that Silicon Valley, sensing an opportunity, had moved into the patient-driven health IT world. “In 2015, Apple released HealthKit, which provides a simple interface for devices including heart-rate monitors and pulse oximeters, creating a de facto data repository under patients’ control,” they wrote. “Companies such as We Are Curious are creating communities of people seeking answers to health questions. Amazon, Microsoft, and Google are collaborating with health care systems to store big data in the cloud.”
The bottom line, Mandl and Kohane said, was that consumers now expect to have their health data available – and sharable.
“A patient-controlled health-record infrastructure can support the development of highly desirable health system qualities,” they wrote. “First, it allows a patient to effectively become a health information exchange of one: as data accumulate in a patient-controlled repository, a complete picture of the patient emerges. If patients can obtain their data wherever they go, they can share them with physicians as needed — rather than vice versa.”
Mandl and Kohane offered a critique of the reasons why the current Meaningful Use standards have been so difficult to implement. “We believe the Meaningful Use program would have been more successful if it had rewarded clinicians for storing data in patient-controlled repositories rather than in EHRs that fragment data across the health care system,” they said.
Within the ongoing conversation around health IT and its implementation in Rhode Island, as well as its use in population health management analytics, one of the challenges is how patients will get to participate in the discussions. And, Mandl and Kohane have posed some provocative questions that need to be integrated into the analysis.