Capturing the data on childhood obesity in RI
Racial, ethnic disparities dominate, with 35 percent of Rhode Island children overweight or obese
PROVIDENCE – With great fanfare, Rhode Island Kids Count released its new data issue brief on the prevalence of children who are overweight or obese in Rhode Island, in a gathering on Friday, March 29, a little more than a week before the 25th annual celebration of the Rhode Island Kids Factbook, scheduled for Monday morning, April 8.
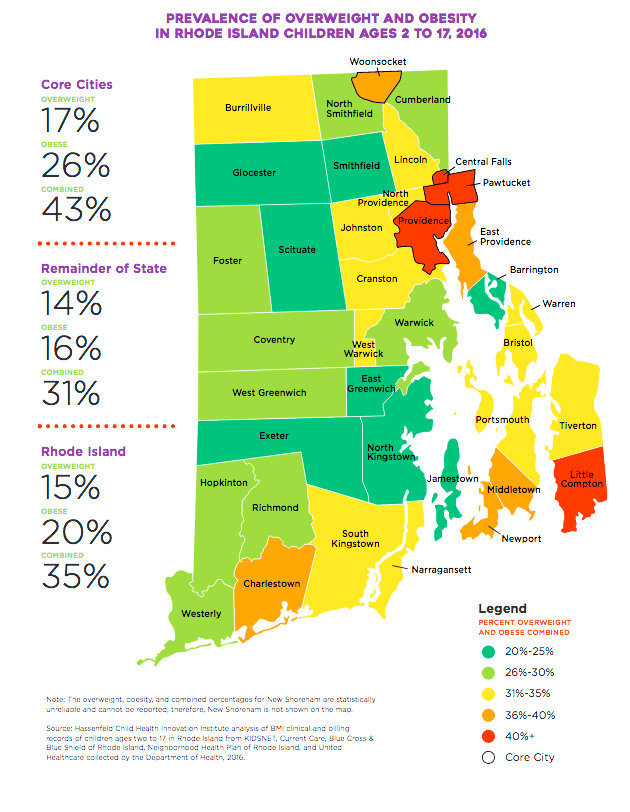
The new issue brief found that some 35 percent of Rhode Island children, ages 2 to 17, based upon data from 2016, were overweight or obese, a takeaway that captured the weighty dimensions of the problem.
The new issue brief also underscored what had been identified as a major gap in health data: the lack of comprehensive data measuring body mass index, or BMI, for children in Rhode Island. The findings contained in the new issue brief, entitled “Childhood Overweight and Obesity: New Data for Rhode Island, represented the efforts of a statewide coalition of providers, insurers, community advocates and agencies to bridge that gap.
The release of the issue brief and ensuing discussion featured opening remarks by Kim Keck, president and CEO of Blue Cross & Blue Shield of Rhode Island, The health insurer had provided financial support for the data project and the publication of the four-page glossy document detailing the findings. Keck praised the importance of the new dataset as a way to begin to measure the impact of the ongoing investment to curb the prevalence of obesity in Rhode Island children, because it puts children at risk for long-term poor chronic health problems.
Keck was followed by a comprehensive analysis of what conclusions could be drawn about the new dataset by Devan Quinn, policy analyst at Rhode Island Kids Count, along with specific recommendations. The recommendations, according to Quinn, included ways to expand and build out the existing database, including capturing data from schools concerning height, weight and age of students. To facilitate that process, one of the recommendations suggested seeking a legislative change that would provide an opt-out rather than an opt-in consent model for collecting children’s health data, to be used on a de-identified, population-based scale by CurrentCare.
Quinn also cautioned about trying to read too much into the analysis around the prevalence of obesity in children by geographic location, saying that the data represented a first cut rather than a deep dive. The data around gender, age, insurance status and race and ethnicity was more robust, she indicated, because it could be correlated with national datasets.
Panel disussion
Following Quinn’s analysis, there was a panel discussion that featured: Ellen Amore, from the Center for Health Data and Analysis at the R.I. Department of Health; Dr. Patrick Vivier, from the Hassenfeld Institute for Child Health Innovation; and Karin Wetherill, from the Rhode Island Healthy Schools Coalition.
The real import of the issue brief, all the members of the panel discussion agreed, was creation of the dataset, which had never existed before. Translated, that effort sought to cull existing health data about children’s body mass index, or BMI, from an amalgamation of data sources.
Those sources included: KIDSNET, the statewide health database on children; CurrentCare, the state’s electronic health information databank; and de-identified insurance claims data from Blue Cross & Blue Shield of Rhode Island, Neighborhood Health Plan of Rhode Island, and UnitedHealthcare.
All this data was then sorted and analyzed by a team from the Hassenfeld Child Health Innovation Institute, in order to determine if the composite mixing and matching of the data sample represented a standardized data representation of Rhode Island. The answer was yes.
The first cut of the data, which correlated the incidences of obesity with race and ethnicity, insurance status, the number of Rhode Island children between the ages of 2 to 17, broken down by city and town, according to age and gender, was just that, the panel agreed: a first cut of the data.
A familiar refrain
The data featured in the new issue brief sounded very familiar. But, it was not until the session was opened up for questions from the audience, and Elizabeth Burke Bryant, the executive director of Rhode Island Kids Count, recognized ConvergenceRI, and thanked him for his previous reporting on the topic, that the realization hit home: ConvergenceRI had covered a preliminary report on the data brief that had been presented to the State Innovation Model Steering Committee, reporting on it in the Aug. 20, 2018, edition. [See link below to ConvergenceRI story, “Mining the golden ore of clinical data.”]
[A quick review of the data in the preliminary report from August 2018 and the current issue brief found most of the findings to be the same.]
ConvergenceRI directed his ‘upstream” question to Vivier, who had done extensive mapping and analysis of lead data and its correlation with asthma, asking: In a similar manner to the work done on lead and asthma, could the high incidence of obesity in Rhode Island perhaps be correlated with potential contamination of drinking water by PFAs, the chemical produced in the manufacture of Teflon? A study conducted in Cincinnati with pregnant women and their children had found correlation with childhood obesity and the toxic chemical, and Joseph Braun, an epidemiologist at the School of Public Health at Brown, had been involved in that study.
Vivier, despite the complexity of the question, welcomed the inquiry. The work on lead, he explained, had created a comprehensive dataset that allowed health researchers to pursue active interventions. The new dataset on obesity in Rhode Island, Vivier continued, was the first step in getting to that next level of analysis and potential environmental links. Vivier also praised the work being done by Braun.
On the ground
Next, a member of the Pawtucket school committee asked about the ways in which agencies and community advocates might focus on the nutrition values in school meals. Some 80 percent of students, she said, received breakfast, lunch and snacks every day. If the desire was to reduce the incidence of obesity in schoolchildren, the focus, she argued, should be on improving the nutrition content of meals, with less sugar content.