Prescription drugs, not utilization, are driving high health costs in RI
New analysis on cost trends reveals that the annual growth in health care cost trends per capita has risen by 4.4 percent from 2016 through 2018, 28 percent higher than the 3.2 percent increase cap on spending
That assumption proved to be wrong, terribly wrong. In Olneyville, for instance, one of the two hardest hit communities when it comes to COVID-19, data from Neighborhood Health Plan of Rhode Island revealed that a high percentage of male residents do not have regular access to a primary care providers – 13 percent among whites, 31 percent among Blacks, and 39 percent for Latinx men, according to Merrill Thomas, the president and CEO of PCHC. “These are the statistics that show that people are not getting care and that there are severe disparities by race and ethnicity,” Thomas said.
PROVIDENCE – When the modern-day brown shirts stormed the U.S. Capitol on Wednesday, Jan. 6, at the urging of President Donald Trump, it was easy to lose track of important health stories occurring, beyond the devastating toll of the COVID-19 pandemic sweeping our country and our state, with 22.2 million people infected, more than 373,000 deaths in the U.S., and 1,916 deaths in Rhode Island – and counting.
• Haven, the Boston-based firm created by three of the wealthiest business titans – Jamie Dixon at J.P. Morgan Chase, Jeff Bezos at Amazon, and Warren Buffet at Berkshire Hathaway – to forge a new approach to redesigning health care, officially folded its tent. The high-profile CEO of the new firm, Dr. Atul Gawande, had departed his position in May of 2020.
The goal of the new venture had been to tame the out-of-control health care costs by focusing on improving the health care delivery to employees while doing a better job of managing the expense. The wealthy trio threw in the towel, without giving an explanation why.
Currently, employer-sponsored health insurance covers about 157 million people in the U.S., according to the Kaiser Family Foundation, as reported by the Associated Press. In 2018, the year before Haven was founded, U.S. health care costs were $3.6 trillion, equaling 17.7 percent of the gross domestic product.
Here in Rhode Island, in February of 2019, with much fanfare, under an executive order by Gov. Gina Raimondo, a public-private compact established a Health Care Cost Trends Collaborative Project, with the goal of setting an annual health cost per capita growth target of 3.2 percent for 2019-2022. [See link below to ConvergenceRI story, “Annual cap of 3.2 percent put on health care costs in RI.”]
The photo of the smiling, buoyant group at the news conference held on Feb. 6, 2019, at School of Public Health at Brown University, when the 3.2 percent cap in annual growth per capita in health care costs was announced, included: Gov. Raimondo [who will soon leave office to join the Biden administration; Kim Keck, the president and CEO of Blue Cross Blue Shield of Rhode Island [who departed her job to take the helm at the national Blue Cross Blue Shield Association; Marie Ganim, R.I. Health Insurance Commissioner [who has since retired]; Neil Steinberg, president and CEO of the Rhode Island Foundation; Dr. Timothy Babineau, president and CEO of Lifespan and Dr. James Fanale, president and CEO of Care New England, the two largest health systems in the state; Dr. G. Alan Kurose, the president and CEO of Coastal Medical; and Teresa Paiva Weed, the president of the Hospital Association of Rhode Island, among others.
The crunching of the data was to be done in partnership with the School of Public Health at Brown University.
Bad news
In the closing days of December 2020, the project’s analysis of trends in health care costs was submitted to the R.I. General Assembly, in a document prepared by the R.I. Office of the Health Insurance Commissioner and the R.I. Executive Office of Health and Human Services. The news is not good.
• The per capita total health care expenditures in Rhode Island rose from $7.001 billion in 2017 to $7.309 billion in 2018, a 4.4 percent increase, 28 percent higher than the goal of 3.2 percent.
• The total spending and trend by service category [net of rebates] showed that retail pharmacy costs had increased 9.8 percent in 2018, the highest trend in increasing costs, to $1.155 billion, followed by hospital outpatient, with the next highest trend in increase cost being driven hospital outpatient services, at 7.2 percent, at $1.254 billion.
• By comparison, the cost trend for hospital inpatient services, fell 0.9 percent, to $1.433 billion.
The shocker
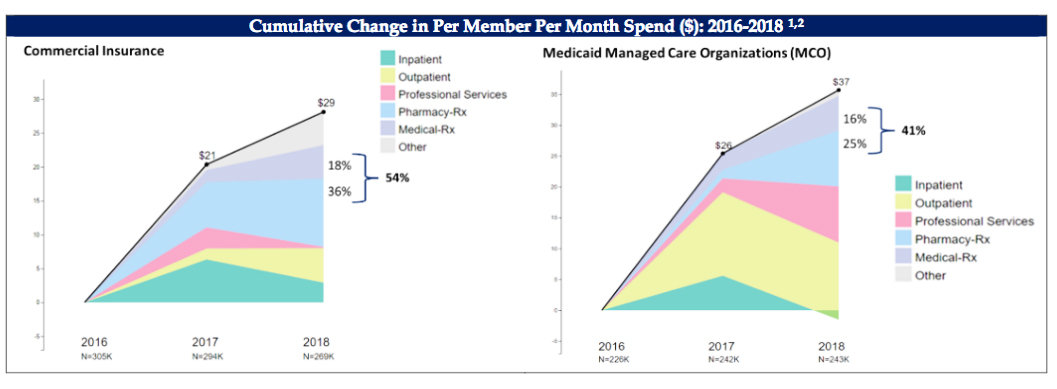
A chart showing cumulative changes in per member per month spend in dollars for the years 2016-2018 produced the biggest surprise. [See graphic.]
• For commercial insurance, costs for Pharmacy RX showed a 36 percent increase and Medical RX an 18 percent increase, for a total increase of 54 percent, a major driver of increased health costs in Rhode Island.
• Similarly, for Medicaid Managed Care Organizations, costs for Pharmacy RX showed a 25 percent increase, and Medical RX showed a 14 percent increase, for a total increase of 41 percent, a major driver of increased health costs in Rhode Island.
Translated, the biggest driver of annual cost trend increases in Rhode Island health care costs was the rising cost of prescription drugs, in both the commercial insurance and the Medicaid markets. The increased costs were not due to increased utilization.
When asked what may be the cause of such a spike in prescription drug costs, one physician suggested that it might be linked to the auto-renewal prescription policies practiced by pharmacies such as CVS and Walgreens, but could offer no evidence.
What the data evidence shows
ConvergenceRI reached out to Anya Rader Wallack, Ph.D., the Associate Director and Professor of the Practice at the Center for Evidence Synthesis in Health at the School of Public Health at Brown University, to get a better understanding of what the cost trend numbers meant.
ConvergenceRI: What did you find most surprising about what the data analyses found in the cost-trends report?
RADER WALLACK: I was surprised that the drug trend was as high as it was, and that it is so clearly linked to price increases, not increases in use. We all suspected this was true, but the evidence is alarmingly clear.
ConvergenceRI: What are the next steps you would recommend to address the rising drug costs identified across all payer platforms?
RADER WALLACK: We will be looking at how we can influence drug prices as a state or as a state in coordination with other states; NASHP [the National Academy for State Health Policy] has provided some models.
ConvergenceRI: With Kim Keck leaving, with Marie Ganim leaving, how do you think that will impact the work of the steering committee?
RADER WALLACK: The work will continue. Patrick Tigue [the new OHIC commissioner] and Michelle Lederberg [the interim BCBSRI CEO] are fully engaged.
ConvergenceRI: In the broader context, what do you make of the decision by the three corporate giants, Amazon, Berkshire and JPMorgan to disband their collaboration, Haven?
RADER WALLACK: Heath care cost containment is freakin’ hard.
ConvergenceRI: What kinds of investment in public health infrastructure would you like to see in Rhode Island?
RADER WALLACK: Not sure. Continued funding of this work [cost trends analysis] is very important.
But the pandemic has also made glaringly apparent the need for constant attention to health disparities. Others would know better where the state has discovered weaknesses in its response.
I think the state and Brown School of Public Health have developed a much closer relationship during this period and continued funding to support that link/work is important.
ConvergenceRI: Is there a way to factor in the way that money has been spent during the pandemic months as part of the next analysis on costs, including the influx of funds from state, federal and loans to hospitals, health centers, and group practices?
RADER WALLACK: We are using the APCD [the All Payer Claims Database] for the Brown analysis, so that money won’t show up in our analyses. However, Bailit [a consulting firm] has gathered data directly from insurers that is more complete but less detailed, and presumably those data will include the pandemic-related funds.
Changes in use [e.g., reductions in use, increased use of telemedicine] that are reflected on claims will show up in our analyses.
ConvergenceRI: What kinds of further data crunching around health care costs would you like to see done? For instance, is there a way to better understand the high drug costs related to specific health care conditions and treatments, such as women's health, diabetes, and mental health and behavioral health?
RADER WALLACK: There is so much we could do on this front. I think the main focus should be where are we paying for care that might be of low value, and where are we paying prices for services where we should not be paying that much.