Truly a beautiful day in the neighborhood
How a volunteer free health clinic – Clinica Esperanza – has reshaped the delivery of health care to the uninsured, under-employed in Providence, during a time of pandemic
Having interviewed Dr. Annie De Groot about her volunteer walk-in health clinic, Clinica Esperanza, and also Dr. Beata Nelken, a pediatrician who opened her practice on Broad Street in Central Falls, both of whom are steeped in the fight to help patients overcome health inequities that have been magnified by the coronavirus pandemic in immigrant communities, I wonder if there is a way to make such discussions more inclusive about the challenges facing women in leadership roles in communities where such health inequities are rampant.
Further, I wonder how the conversation would change is environmental writers and scientists, such as Rebecca Altman, working on a book about plastic, “the Song of Styrene,” and Kerri Arsenault, whose book, Mill Town: “Reckoning with What Remains,” talking about the way that paper and plastic is a thread of environmental pollution that inhabits our lives, our families, our rivers and our own bodies, were to become part of the conversation.
PROVIDENCE – Writing about the success of Clinica Esperanza, a volunteer medical clinic operating in the heart of Olneyville, which recently was awarded $315,000 by TD Bank’s Ready Challenge, is an exploration into how a neighborhood has begun to reinvent itself in the midst of a pandemic, challenging the status quo when it comes to health care.
In a recent interview with its volunteer medical director, Dr. Annie De Groot, and with Frank Casale, the regional vice president at TD Bank, the conversation captured so much of what has not been reported in the last year when it comes to health care in Rhode Island: what De Groot accurately described as uncovering “the size of the iceberg in Rhode Island” when it comes to the large unmet health needs in the state, made starkly more visible by the pandemic.
You see, for much of the last decade, Clinica Esperanza, the “Hope Clinic,” has served the uninsured – patients who lack health insurance, including many hard-working, Spanish-speaking residents, many of whom are immigrants.
[Editor’s Note: ConvergenceRI has frequently reported about the work of Clinica Esperanza. It was featured in a story about the 2018 Health Equity Summit. At that time, Clinica Esperanza said it was serving more than 2,000 patients a year, mainly Central and South American immigrants, 60 percent of whom spoke Spanish as their primary language and 75 percent of whom reported incomes of less than $15,000 a year.
As ConvergenceRI reported: “The focus of much of the culturally appropriate care delivered is on nutrition education, cholesterol/blood pressure/glucose checks, primary care and vaccinations. Through what is known as the “Bridging The Gap” program, which includes quarterly visits with a primary care provider and participation in a health education program, patients’ use of emergency departments was reduced significantly compared with Medicaid patients.”
The story continued: “One of the goals of the program is to manage chronic diseases before they become emergent or incurable, improving the quality of life and lessening the burden on local hospitals and ERs to provide charity care.” See link below to ConvergenceRI story, “Eyes on the prize; 2018 health equity summit draws 750.”]
For sure, Clinica Esperanza is not alone in its grassroots efforts at the neighborhood level – which also has featured the good work by ONE Neighborhood Builders, the Providence Community Health Centers, the Sankofa Initiative, and the Rhode Island Public Health Institute, among others, to address the issues around health inequities.
But Clinica Esperanza has been among the most consistent, perhaps, in pushing back against the status quo when it comes to health care delivery in Rhode Island – developing a cost-effective program of providing basic primary care to those outside the mainstream of the health care delivery system in the state.
The disastrous spread of the coronvavirus pandemic, which has now killed some 500,000 people in the U.S. during the last year and sickened more than 28 million, blew up the prevailing assumptions that the health care delivery system had things under control.
Clinica Esperanza has been operating for the last 13 years, often dependent on the kindness of neighbors and philanthropic grants, to serve a burgeoning population of people who checked all the boxes for “unmet health needs” – unemployed, uninsured, Spanish-speaking, and lacking access to primary care.
In the interview, De Groot described how the pandemic had helped to suss out the size of the health care unmet needs iceberg in Rhode Island.
“During the pandemic, as you can imagine,” she explained, “even with going to telemedicine, even with limiting visits, we’ve actually had an increase of 130 percent [in new patients], in terms of new patient visits to the clinic, and that’s partly in relationship to the fact that we opened a COVID-testing site.”
You may wonder: How big was the demand for testing? The answer provided by De Groot did not take an advanced degree in health administration or a high-priced business consultant from Boston Consulting Group to interpret the data. It has been huge.
“The Clinic’s COVID testing site tested more than 3,500 people between April and December of 2020,” De Groot told ConvergenceRI. “On average, about 25 percent of those people were COVID positive. And, 66 percent of those people were uninsured, and they were new patients to us. We did not know them before this.”
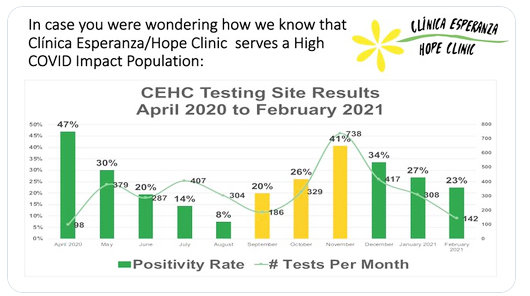
Let that sink in for a moment: The testing site run by Clinica Esperanza, separate from the state-operated sites, tested on average 400 people a month. Two-thirds of the people tested were “uninsured.” One-quarter of the people tested – some 900 people, 25 percent – tested positive, a clear marker of how wide the community spread of the virus has become. And, most were “new patients” – people who had not been known to clinic before. [See second image, a graph detailing the most recent data of COVID testing by the clinic.]
“So, actually having the COVID-testing capacity enabled us to uncover the size of the iceberg in Rhode Island,” De Groot said. “Which is actually how many people in Rhode Island have no health insurance.”
Community heroes
The interview with De Groot and Casale, TD Bank’s regional vice president, revealed the extent to which a critical news story has gone unreported by the Rhode Island news media. Further, it highlighted the philanthropic investment by a major bank in the community-driven volunteer health clinic that is reshaping how a Providence neighborhood is redefining issues of health equity.
Here is the ConvergenceRI interview with Dr. Annie De Groot and TD Bank’s Frank Casale, describing the iceberg of Rhode Island’s unmet health needs and the innovative solutions being delivered – outside of the narrow lens aperture of most news media in Rhode Island.
ConvergenceRI: How did TD Bank get connected with Dr. De Groot and Clinica Esperanza?
FRANK CASALE: First, congratulations to Annie and her team for being a TD Ready challenge winner, one of only six in the United States.
What happened, Richard, is that we have at TD Bank a TD Ready commitment and a TD Ready Challenge. The TD Bank Ready Challenge acts as a springboard for us to invest in social innovation, to establish and identify solutions to specific issues.
Each year, we ask some of the brightest minds in the not-for-profit world to respond with their proposals to help address growing problems within society.
So, those applications, if you will, those requests, come in, and we review them all, and keep narrowing them down. And, that’s how we find such great [programs] such as Clinica Esperanza.
We found Clinica Esperanza when they applied for the TD Ready Challenge.
ConvergenceRI: There are a lot of things to like about what Dr. De Groot is doing with her team at Clinica Esperanza? What specifically did you find that was innovative and ready for investment by TD Bank in the work of the clinic?
CASALE: The TD Bank Ready Challenge is part of the TD Ready commitment. The TD Ready commitment is basically focused on four interconnected drivers that change the community. They are: [promoting] financial security, having a vibrant planet, connecting the communities, and promoting better health.
They are the pillars – the meeting of unmet health care and health education needs of a predominantly immigrant, uninsured, Spanish-speaking population in Rhode Island, was something that was very interesting to us.
They do God’s work at their clinic, taking in uninsured folks, taking care of people who have lost their jobs, and who have lost their health insurance because of that. And that disproportionately affects low-income communities served by the clinic.
And the demands have increased, obviously, with the intensity of the pandemic.
ConvergenceRI: Annie, how will the grant enable you to expand the clinic’s work, providing non-urgent medical care for patients who are uninsured?
DE GROOT: First, I want to give gratitude to TD Bank for supporting this project. It’s really very exciting. And, to Morgan Leonard, who is the new director of clinic operations, who wrote the proposal.
The clinic, as you know, is a walk-in clinic that was set up in 2012-2013, initially with support from Blue Cross Blue Shield of Rhode Island, to divert people away from the emergency room.
The concept was actually that people were going to the emergency room and they were getting bills, and that was harming their credit worthiness because they couldn’t pay those bills. And, they were actually [seeking care] for things like colds, or back pain, or rashes, or sexually transmitted diseases, [conditions] that could easily be treated in a walk-in-clinic, but they didn’t have access to one.
It was also partly state Sen. Josh Miller’s idea. If you remember, as I ‘m sure you do, Richard, at the time, Sen. Miller was trying to create an emergency room diversion program from patients who were being sent to the drunk tank. [Editor’s Note: The pilot diversion program, which ran for a year, was abandoned after it proved impossible to transfer patients to health insurance to pay for the diversion effort, because too many of the patients were undocumented immigrants.]
We found that, in terms of cost savings, since we started the clinic, we were saving local emergency rooms more than $500,000 a year.
[Editor’s Note: The data results were documented in a study published by the R.I. Medical Journal, “Bridging the [Health Equity] Gap,” in November of 2018. “The overall savings from the emergency department diversion aspect of BTG could be as high as $781,122 annually if the program were to be expanded to 8,000 uninsured Hispanics, statewide,” according to De Groot.]
So, being fearless, we actually went to one of the local health care system providers and said: “Why don’t you give us $300,000 a year and then we’ll be saving you $200,000 a year?’ That didn’t go over well, as you can imagine – even though it made perfect sense.
We actually have been really struggling to support this project.
ConvergenceRI: Who were the people who were uninsured, who were seeking out testing for COVID?
DE GROOT: A lot of those people, as you can imagine, are young. Many are usually healthy, but they were obviously getting sick with COVID. We were able to take care of them, using telemedicine initially.
We also worked with local projects, such as the Elisha project, and we were able to bring food to their houses, so that they didn’t have to go out to shop for food.
And, also, with help from United Way of Rhode Island, the Rhode Island Foundation, and the city of Providence we were able to give them cash cards to purchase groceries when they were feeling better, because obviously, they couldn’t go back to work, work was shut down.
We really provided a safety net for the safety net.
But now, these patients are our patients, so the award from TD Bank will give us the opportunity to take care of these patients, in an ongoing manner, over the next year, and hopefully, beyond that, because of the support that they are giving to the clinic.
ConvergenceRI: If you were able to get access to vaccines, are you prepared and would you be able to then vaccinate these same patients?
DE GROOT: Absolutely, and thank you for asking that question, Richard. And, Frank, you’ll be happy to know that we are setting up to be a vaccine site.
We have jumped through almost all of the hoops; it has been quite the exercise. We now have our state-approved refrigerator. The state has inspected our site. We have the proper social distancing in place. We have signed up for the mod vaccine scheduling service.
All we’re waiting for right now are the actual vaccines. We have a list of over 300 patients who are all over 75 years old, and uninsured, who come from our patient population. First, we will be setting up appointments for those people. And then, we will be opening to the general public for those who are over 75, and then as the Rhode Island prerequisites roll forward, for those over 65 in the same population.
That’s the exciting news for this week.
ConvergenceRI: Wow.
DE GROOT: I’m not sure exactly when we will open, Richard. I’m hoping that it’s Thursday, Feb. 18 [The interview took place on Tuesday morning, Feb. 16.]
The vaccination site is in a different location, because we were so busy with COVID testing that it was impeding our clinical care. We were able to get funding through the federal CARES Act to open a separate, COVID testing and vaccination site, which is located in Eagle Square. We have a big space, and we have a beautiful mural that talks about health in Guatemala.
[Editor’s Note: Despite the clear messaging on Clinica Esperanza’s website, a number of Rhode Islanders who were not 75, and who were not uninsured, attempted to jump the line, demanding that they receive vaccines, creating a stir.]
ConvergenceRI: How important is it, do you think, for people to understand that the unmet needs didn’t come about just because of the coronavirus pandemic? But rather, you are addressing deep-rooted problems in the community around health equity that have been magnified by the pandemic?
DE GROOT: Absolutely. I think everyone in the U.S. is well aware that the people who are at highest risk are disproportionately Latino and African American. Our [client] population is predominately Latino; we have one of the biggest Guatemalan populations in the Northeast in Rhode Island.
Most of our patients are Spanish speaking; they are uninsured, they are working low-wage and very transient jobs, and they do not have access to health insurance.
So we have been providing that safety net for many years now. We have been open 11 years in this current location, but actually we have been open for 13 years.
This is a population that is at high risk, partly because of language barriers, but also because of a lack of health literacy. A lot of people are unfamiliar with the basic concept about viruses and about how they are transmitted. There is a lot of education that has to occur.
Many of our clients live in multi-generational and multi-family households. Many of our patients live one family to a room, in three-bedroom apartments. It’s really quite crowded; it’s often impossible to do any kind of social distancing.
And so, that is why, when one person is infected, usually, it impacts 10 to 15 people who live in the same house.
ConvergenceRI: How are you communicating with folks? Is it mostly done through telehealth? Has the wire mesh network that has been built out by ONE Neighborhood Builders been helpful?
DE GROOT: I’m not aware that that has been impacting our patients. We usually reach them by cell phone. And, it’s a constant battle, because they are constantly switching their phone numbers.
We have a network of about 2,000 cell phone numbers that we can reach out to our patients. We have test messaging system called Care Message that allows us to send text messages in English and in Spanish, and get answers back, with “Yes” or “No” answers.
We’ve determined that 80 percent of our population is ready to get vaccinated – when we asked them if they were ready. So, that’s the exciting news. People in this population [who we serve] are ready to get vaccinated, because they have seen the devastating effect that COVID has had on their colleagues and their families.
There is really no way of reaching them other than text messages. We also do some outreach through Facebook. One of our board members, Dr. Pablo Rodriguez, who runs a talk radio show, but on Facebook, called “Rhode Island Informa,” he’s been talking about vaccinations.
We also have our own Facebook page, through which many of our patients have reached out to us, so they have actually scheduled appointment for COVID testing through Facebook. That has been a way that we have been reaching our patients as well.
Television doesn’t work. As you know, there is no local television station in Spanish.
There’s really no other way of reaching these individuals, other than by word of mouth. Beginning when we first opened the clinic, word of mouth has been the best way to reach people. We have asked them, over and over again, “How did you hear about us?” They answer; “A friend of mine told me.” That is universally what they say.
ConvergenceRI: How do you feel that your clinic strengthens the concept of “neighborhood?”
DE GROOT: Do you want to address that question first, Frank?
CASALE: At TD Bank, we are really focused on aspiring to make a difference in the lives of the most vulnerable in our communities. We have a lot of folks who work for us, me included, that serve on a number of various boards, such as the Rhode Island Food Bank and Meeting Street. It’s just what we do; it’s in our DNA.
Especially as TD Bank members, we are committed to the community. And, we want to make a difference in the community. And, what better way to do that than to support organizations and folks such as Annie, Morgan, and their team. We are very proud to be partnering with them.
DE GROOT: There are some very important aspects of community that we address. First of all, we reach communities that are hard to reach. At Clinica Esperanza, over the years, we have built trust in the community of immigrants, and with Spanish-speakers who live on the West Side of Providence.
But we also have patients who come to us from all over the state, people come to us from as far away as Block Island and as close by as Central Falls, to our clinic for their health care.
In that sense, we have built a network in the community to provide a safety net to people that would otherwise really have no other access to health care.
In addition, I think we do something that is very, very important: We bring neighbors together to help neighbors. We are a volunteer-run clinic. I’m a volunteer. I’ve always been a volunteer at the clinic.
[Editor’s Note: In her “day job,” De Groot is the co-founder, CEO and CSO of EpiVax, Inc., one of the pioneering biotech firms in Rhode Island, which has developed its own proprietary immuno-informatics data software, and which is involved in research in developing vaccines across a number of cutting-edge health threats, including coronavirus.]
We benefit from the good will of the community, and having a clinic like this makes it possible for people to contribute to the well being of their neighbors.
Because I can see how much the community in Rhode Island, and that includes TD Bank and all of other supporters, how much our community cares for each other. I think that is one of the most important messages. In this pandemic, we do care about our neighbors and for each other, and we do reach out.
It’s really been wonderful to be able to be see how our work changes lives, not only for the patients, but also for the volunteers.
ConvergenceRI: What questions haven’t I asked, should I have asked, that you would like to talk about?
CASALE: We are committed to the community. The TD Bank Ready Challenge will grant some $20 million this year, with a commitment to invest $775 million by 2030. It is a philosophy, it is a strategy, and it is a commitment.
DE GROOT: I think it is important to talk about this effort in the context of the entire city and the entire state.
Rhode Island has really been the beneficiary of immigration by a group of some of the most hard-working, morally and ethically upright people. I am talking about the Guatemalan people and other immigrants from Central America who have come here to work hard and to make a better life for themselves and their children.
For me, it has been a wonderful experience, working with the immigrant community. I feel it is important to get back to a place where we appreciate the importance of immigrants in our community, the energy that they bring, and the investment in their children. So many of the young workers at our clinic are first generation immigrants, children and dreamers who are working very hard to make a better live for themselves and their kids.
I commend TD Bank for their investment in the West Side of Providence through Clinica Esperanza, and I believe we will strengthen the entire city and the entire state through this effort.