Dear Abby, Dear Abby
Finding answers to the difficulties encountered in health care
WARWICK – As a reporter, one of the things you always do is maintain a list of contacts – people whom you can call and, in turn, people who will call you, to ask questions about something that either happened to them or to a friend.
Last week I hit the jackpot. Three different people, from three separate walks of life, called me up to ask my help in deciphering the difficulties they had encountered with the health care delivery system in Rhode Island.
It made me think that I should consider offering an advice column as part of ConvergenceRI’s standard fare of reporting. The fact is this: Difficult encounters keep increasing, often leaving patients in the lurch. The patients are often frustrated and angry, because there is no good place to turn for answers or resolution. Who are you going to call? Ghostbusters?
The first call came in from a middle-aged person who, all of a sudden, had encountered great difficulties in trying to get her prescriptions refilled. No one – not her health insurance company, not her doctor, not the hospital system through which she had been receiving care on an outpatient basis, could explain what was happening to cause her inability to obtain her medicine. “It would make a good story,” she said, asking me to look into what was going on.
Without digging too deeply into her situation, it was clear that she may have fallen into the rabbit hole created by a cyber-security hack of Change, a for-profit pharmacy benefits manager that had been acquired by UnitedHealthcare, disrupting the ability of pharmacies all across the nation to dispense medicine. Once again, the reporting of Moe Tkacik in the Prospect, has led the way in trying to untangle the facts behind a nation and its doctors and patients caught in pharmaceutical purgatory.
“Last Thursday [March 7], the medical colossus UnitedHealthcare applied for an emergency exemption that would fast-track its takeover of a medical practice in Corvallis, Oregon, in a letter warning regulators that the practice might close its doors if the merger were not approved right away,” Tkacik wrote in her story, “UnitedHealth exploits an ‘emergency’ it created.”
Tkacik’s reporting continued: “Although the specific reason for the exemption request is redacted from the publicly posted version of the application, a clinic insider says the ‘emergency’ is the same one that has plunged thousands of other health providers across the nation into a terrifying cash crunch: the weeks-long outage of UnitedHealth’s Change Healthcare clearinghouse and claims processing systems, which has halted the flow of information that enables physicians, hospitals and other health care providers to get paid for their work.”
What had caused the cash flow shortfall? The answer, according to an insider source, an employee of the Corvallis Clinic, told Tkacik: “Our claims processing goes through [Change], so all of a sudden there was no money coming in,” the insider, an employee of The Corvallis Clinic who did not want to be identified for fear of jeopardizing the transaction, told the Prospect.
The clinic’s shareholders, who include more than half of its 110 physicians and one of its behavioral health providers, worked without pay last week in order to “scrape together enough money to pay the staff,” the insider said, but on Thursday the shareholders explained that they weren’t sure they would be able to open the doors Monday without an emergency cash injection. ”They’re praying that the sale’s going to go through and that Optum will front them the money.”
Translated, it sounds a bit like the old joke about the definition of chutzpah: a young man pleading for mercy from the court because he is an orphan, having murdered his parents.
In Rhode Island, as reported by Boston Globe, “Change Healthcare, a national medical claims company with a presence in Pawtucket, took its systems offline after a cyber attack that affects R.I. Medicaid and AIDS Drug Assistance programs.”
After the cyber attack, the Globe reported, “Rhode Island Medicaid was temporarily unable to pay pharmacies for filling prescriptions for its members, officials said.”
The Globe further reported: “Folks may have gone to get their presecriptions and couldn’t get them, or they were told that they had to pay out of pocket,” EOHHS spokesperson Kerri White said. “But thankfully, we brought a new system online and requested pharmacies to follow the pharmacy provider manual and provide prescriptions up to 30 days. So we hope people are able to get their medications.”
Free-flowing fraud?
Another call came last week from a resident who had been referred to me through a reporting colleague. The resident had been the target of an apparent Medicare fraud, allegedly charged some $18,000 for catheters through a physician that was said to be part of the Lifespan network; it is a product the resident said he had never ordered.
The resident said he had had made his way through various portals to seek help and protection. They included: the U.S. attorney’s office, the R.I. Attorney General’s office, Lifespan, UnitedHealthcare, the doctor’s office allegedly involved, and the Medicare fraud hotline. The resident, who worked in law enforcement, said he was worried that there had been an apparent breach of the insurer's data security.
The patient’s suspicions about data threat may have been correct, it turns out. A few days after the patient’s phone call, ConvergenceRI happened upon a story in The Washington Post on Wednesday, March 6, by reporter Dan Diamond:
The story began: “House Republicans on Wednesday demanded that federal health officials address an alleged Medicare fraud ring estimated at more than $2 billion. Health-care groups warn that the scheme has ensnared hundreds of thousands of patients and continues to expand.”
The story continued: At least 10 companies are linked to an unexplained surge in bills for intermittent urinary catheters, low-cost devices used to relieve urinary incontinence, according to interviews with health-care officials, physicians and patients and documents obtained by The Washington Post. In recent years, clinicians and other medical providers had billed Medicare, the federal health insurance program for older Americans, for about $150 million worth of those catheters annually, on behalf of 45,000 patients. That abruptly spiked starting in late 2022.
The National Association of ACOs, a health-care organization that helped identify the alleged fraud, warned members in February that at least $2.8 billion in claims to Medicare were linked to the catheters last year alone, citing its review of federal billing data. That represented a roughly 30 percent increase from the group’s earlier estimate.
An earlier story by the Washington Post, published on Feb. 9, had explored the details behind the alleged fraudulent scheme.“We’ve just never seen anything like this nationally,” said Clif Gaus, CEO of NAACOS, who said his organizations first spotted and reported the billings to federal officials last fall. Gaus’s team estimates that Medicare was wrongly billed about $2 billion for the catheters in 2022 and 2023.
The story continued: “Gaus said he was concerned the companies behind the surge in catheter bills were using real patients’ data to order medical products that the patients did not want or need.
“Where do you get half a million [Medicare] beneficiary names and ID numbers?” Gaus asked. “There has to be a breach somewhere in the health-care system,” suggesting several possible sources, such as health-care records or consumer data.
Dear Abby, Dear Abby
With all the ongoing reporting, nationally and locally, about health care – 25 new bills proposed by the Senate President on March 5, the focus on women’s health care in the Presidential election, and the continuing reverberations of what will become of Steward Health Care in Massachusetts – it was easy to miss the data evidence presented by the Woonsocket HEZ, focused on the homeless population in northern Rhode Island communities they serve.
The HEZ report was presented to the Community Partnership Task Force on Homelessness in Woonsocket. Given that there were reported to be some 800 individuals, families and children residing “outside,” the situation is predicted to get even worse, according to community advocates.
What were presented were two data trends of enormous importance, in ConvergenceRI’s opinion. The first dataset concerned the transit problems facing those residents confronting the risk of homelessness, and the length of the distance and travel time they faced in trying to access shelters – whether by driving or by public transit – often found to be in hours. Translated, it is a complex, complicated path for those at risk of homelessness to reach shelters or to reach medical services,
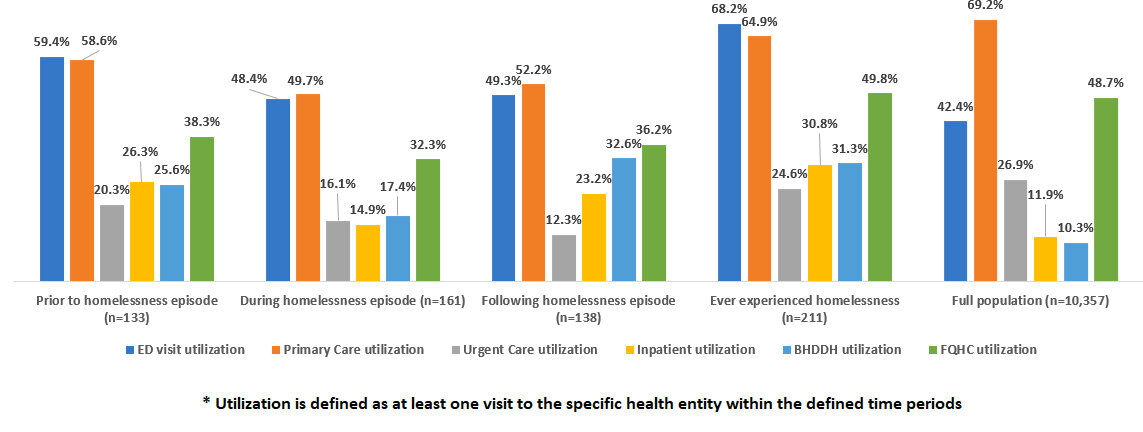
The second data report looked at utilization of health services, broken down by needs, for the clientele being served.
The question is: How does the state begin to have a conversation that connects health care to public transit to homelessness? Is it merely a conversation that is an add-on to the problems uncovered by the Washington Bridge repairs? Is it something that the Governor’s Task Force on Overdose Prevention and Intervention should look into and invest in finding solutions, because the inability to access treatment and services is linked to the inability to access behavioral and mental health services across all ages and demographics? Imagine if the state were to invest in a plan of transit innovation – a bus service connecting patients and medical services and shelters – as an innovation ecosystem enterprise.
ConvergenceRI reached out to the health equity zone in which ONE Neighborhood Builders in Olneyville serves as the backbone agency coordinating the efforts, speaking with Kyle McKendall, vice president of resource development and communications for the community development agency. ConvergenceRI shared the report by the Woonsocket HEZ, asking whether the data trends reflected in the populations served in the Woonsocket region were similar to what residents in Olneyville and the surrounding neighborhoods were experiencing.
The answers were, in turn, provided by Anusha Venkataraman, the managing director of ONE Central Providence.
ConvergenceRI: Do residents served by the HEZ managed by ONE neighborhood builders encounter the same kind of transit barriers?
VENKATARAMAN: Transportation is a statewide issue. The topic of transportation has consistently been mentioned as a challenge or barrier by those who live and work in Central Providence during our working group meetings. Inadequate, inaccessible, or unreliable transportation creates barriers for residents from accessing quality and rewarding work, safe and affordable housing options, educational opportunities, and health care resources.
ConvergenceRI:What kinds of transit solutions are needed in your neighborhoods to access health care and support for housing issues?
VENKATARAMAN: Solutions to the challenges we see should be systemic and should measurably improve day-to-day life for those severely impacted by the challenges and inequities. Solutions are likely to fall into these buckets:
- Adequate investment in public transit.
- Investment and improvements to the places where people access public transit.
- Centering of community voice and perspectives in making decisions about dollars, service, and related investments.
For example, during our Nine Neighborhood Fund initiative, the state’s largest participatory budgeting project where residents got to decide on how to invest $1 million in their neighborhood, residents chose to advance the “Improving Our Bus Stops” project.
This project will direct $132,000 to add seating, lighting, and additional amenities near approximately 4 bus stops that currently do not have shelters in the neighborhood.
ConvergenceRI: Has ONB created a dataset similar to what has been created in Woonsocket to identify the transit barriers?
VENKATARAMAN: We have not formally created a transportation-focused initiative but continue to advance important conversations on the topic within all of our working groups and ongoing discussions.
ConvergenceRI: What kinds of collaborations would you suggest might be possible to invest in for the Olneyville neighbors?
VENKATARAMAN: Through the Nine Neighborhood Fund process, Central Providence communities have demonstrated that residents are important partners in improving our transit infrastructure. Participatory budgeting, as a process, can create stronger government-community partnerships and can build overall trust.
Another example of collaboration we’re a part of is the DOT Thriving Communities technical assistance program. We are working alongside partners from the City of Providence Planning Department, Smith Hill Partners Initiative, and Providence Resilience Partnership to advance the implementation of the Smith Street Revitalization Plan by identifying resources to invest in community infrastructure and increase pedestrian and bicyclist safety.
Asking advice, getting answers?
As ConvergenceRI was writing this story, a pitch arrived in the Junk email folder for a new service, “DoctorAI,” which promised to “transform your health journey with Doctor AI.” The sales pitch went like this: “Why wait for answers? Your immediate diagnosis with DoctorAI.”
The copy for the come-on reads: “As we navigate the intricacies of modern healthcare, the difference between traditional medical consultations and the innovative solutions offered by Doctor AI has never been clearer.”
“Really?” to once again quote one of the state’s hardest working reporters, Steve Klamkin.
The problem, of course, is that medical diagnoses are often problematic – reading symptoms and signs and tests about the human condition and our relative health and wellness is often an inexact science. At the core is the confidential relationship between the provider and the patient. Machine learning and AI cannot replace the relationship between the patient and the provider.
Still, there is a need to be able to talk about the problems of modern life, and the need for a “connectedness” to the neighbors and community in which we reside. How do we do that?
At the root of human interactions is storytelling. Our personal stories are our most valuable possessions. Sharing them is what makes us human, creating a place-based connection in our lives so that we have a place where we belong. At its essence, ConvergenceRI is about storytelling and sharing stories, creating a narrative that resonates with the reader.