Overcoming resistance
One-on-one with Laurie Gunter Mantz
The Boston Globe, for instance, recently conducted a survey, asking if respondents’ use of the following online news sources had changed in the past year.
Listed were The Providence Journal, The Valley Breeze, GoLocal Prov, BostonGlobe.com, Providence Business Journal, and Providence Monthly.
Inexplicably left off the list were the Providence Business News, ecoRI, ConvergenceRI, and UpriseRI, and RINews Today, among others.
The editor of the Boston Globe edition in Rhode Island, Lylah M. Alphonse, said that “the goal was to look at general news sources, not topic-specific ones,” in response to criticism from William Hamilton, an editor at PBN.
The failure to recognize the good news reporting done by others in the market – and to exclude them from surveys – is illustrative of why so much misinformation exists within the state's media space, unfortunately.
PART Two
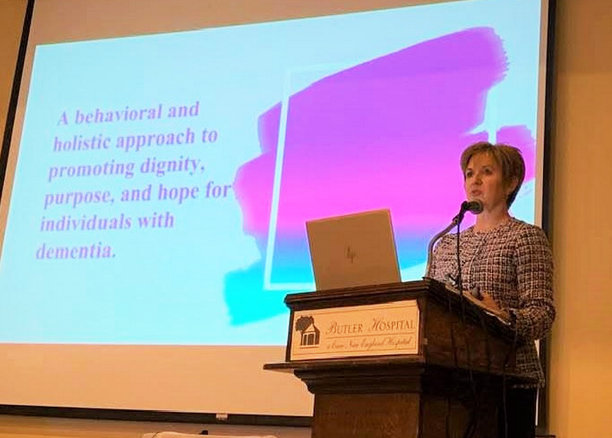
PROVIDENCE – Here is the ConvergenceRI interview with Laurie Gunter Mantz, which follows PART One, an op-ed she wrote about why dementia is not a disease.
ConvergenceRI: Do you know how many people living in Rhode Island have been diagnosed with dementia?
MANTZ: With Alzheimer’s, the numbers are approximately 26,000, 27,000 people. But there are multiple diseases diagnoses that can cause dementia. Currently, they don’t keep statistics on the other diseases. We also know there are thousands of individuals undiagnosed. That is part of the problem.
ConvergenceRI: What kind of research is being conducted in Rhode Island about neurocognitive disorders and their connection to the COVID pandemic?
MANTZ: There is a lot of research happening in Rhode Island. We’ve got centers of excellence, and a new program just established at Brown University. To my knowledge, tt is not looking specifically at how COVID has impacted individuals living with dementia.
But, they are looking at different ways that they can help people improve their cognitive functioning and maybe even delay the onset of dementia. Research has shown we can prevent some of the cognitive loss that we see with neurocognitive disorders.
ConvergenceRI: Is there resistance from the medical establishment about how best to treat dementia? Are you considered an outlier in your work? Where is the pushback?
MANTZ: Yes, there is some resistance. It is hard to understand why, from my point of view. Some doctors and health care professionals are resistant to getting the education, so they do not always understand the differences.
They are overwhelmed and have so much to do, especially since COVID, that they can’t add more onto to their plates; that is my interpretation and impression.
ConvergenceRI: Is there too much emphasis being placed on drug development and not enough on cognitive therapies in the treatment of dementia, in your opinion?
MANTZ: This is definitely my opinion, yes.
ConvergenceRI: Can you explain why that is your impression?
MANTZ: Research has shown there is so much that we can do, with education to teach people how to manage the different symptoms that result in dementia.
But, everybody is looking for the fast, magic pill. And, that’s the same with COVID. People just want a pill that is going to make it all go away. It is much harder to get people to recognize that it takes a lifestyle, a routine, and regular intervention to make it so that the person living with dementia can live as independently, and with the best quality of life for as long as possible.
ConvergenceRI: Is your work considered controversial?
MANTZ: No, I don’t think it is controversial. Typically, people seek me out, and seek out some of the things that I do, when they just can’t figure anything else out. They need more resources and support It is very frustrating for care partners and for those living with dementia when they do not feel heard.
That is where the push for earlier diagnoses is so important. Earlier intervention definitely provides a better quality of life.
ConvergenceRI: How do you view the current structures of skilled nursing homes and their ‘memory’ programs as it relates to the kinds of work that you are doing?
MANTZ: One of the things that I find is staff believe that the only people that have cognitive issues and need specialized memory support are the ones that are in their special care units.
That is not the case. There are plenty of people who are living in the facilities that still need additional support. All staff need to be educated,
ConvergenceRI: Is there a way to bridge the gap, between what you are saying and what the skilled nursing facilities are doing?
MANTZ: Education. There is a major staffing crisis going on throughout health care right now. Unfortunately, the thought is, you can’t take the time to train people because we don’t have enough time.
But well-trained staff will provide efficient and effective care, thus giving them more time, in the long run. It is that Catch-22 situation.
ConvergenceRI: Is part of the problem related to changing the approach to dementia related to the fact that there is often too much reliance on the expertise of doctors? I may not be phrasing the question well.
MANTZ: In general, the older generation, say 70 and older, tend to believe that the doctors are the experts and don’t question that.
Whereas the younger generation is now getting to the point where they are starting to advocate for themselves. Unfortunately, many doctors are not trained in dementia care or diagnosis.
Too often, we are still hearing doctors say, “Dementia is just a normal part of aging.” But it’s not.
So, we need to make sure that all health care professionals are getting education in neurocognitive disorders that cause dementia. We have some of that problem with nursing, too, particularly with people who have been in nursing for a long period of time. The newer professionals, the younger professionals, have a little bit more of an awareness that there are treatable conditions that can look like dementia but where we can actually reverse the situation, like with Lyme disease, or with hearing loss.
It is getting people to change understand the stigma; dementia is not a normal part of aging. Not everybody over the age of 55 is going to get dementia, and just because you are getting older doesn’t mean it is inevitable.
We can treat the symptoms and improve the quality of life with early and accurate medical care.