Reinvention of Medicaid continues to evolve
A new line-up of managed care organizations appears to be in the works
For all the efforts to discern a competitive edge in the current political landscape, I would be curious to know where health care places in a survey of the most important issues, broken down by demographics. My suspicion is that successful candidates will be those that can connect with voters around health care issues.
PROVIDENCE – The roster of private contractors designated to serve as managed care organizations under the R.I. Medicaid umbrella appears poised to undergo significant changes.
Blue Cross and Blue Shield of Rhode Island said it had responded to a Request for Information issued earlier this spring by the R.I. Executive Office of Health and Human Services.
“It would be premature to provide any additional comment until the RFP is released and we’ve had time to review it,” said Gail Carvelli, spokesperson for Blue Cross. “Responding to the RFI does align with our vision to passionately lead a state of health and well-being across Rhode Island for all Rhode Islanders.”
Another apparent respondent to the RFI is Molina Healthcare, a Fortune 500 company headquartered in Long Beach, Calif., according to a number of sources. In September, Molina Healthcare was named Florida’s top-ranked Medicaid HMO, according to the company’s website.
“R.I. EOHHS is preparing to release a procurement for managed care contracts,” said Kerri White, spokesperson for EOHHS, in an email to ConvergenceRI. The timeline for the procurement is still be determined, according to White.
“We welcome all bidders interested who can meet the terms of the RFP to provide the best service for our members and Rhode Island taxpayers,” White continued.
The current roster
Currently, there are three private contractors that have been operating in Rhode Island as managed care organizations for Medicaid members, serving roughly one third of all Rhode Island residents.
• Neighborhood Health Plan of Rhode Island serves roughly two-thirds of the market; UnitedHealthcare serves nearly one-third of the market; and Tufts Health Plan serves the remaining portion of the market.
Tufts Health Plan was designated as a managed care organization in 2016 as part of the Reinvention of Medicaid, following the receipt of a $129.7 million in new federal funds from the Centers for Medicare and Medicaid Services.
With the potential entrance of both Blue Cross and Blue Shield of Rhode Island along with Molina Healthcare as competitors into the MCO marketplace, the yet-to-be answered question is: Will the new potential entrants force Tufts Health Plan and UnitedHealthcare out of the market?
Roadmap in Year 5 for Accountable Entities
White also provided the link to the “Year 5 Roadmap and Sustainability Plan,” effective July 1, 2022 through June 30, 2023, which offered a detailed look at how the agency is proceeding with plans to implement a new Long-Term Services and Support Accountable Entity program with its own alternative payment model, with the goal of developing “a pay-for-performance model focused on services that would enable long-term services and support eligible populations to live successfully in their communities.”
Translated, the approach marks the latest effort by the state to socially engineer a way for residents to stay in their homes longer, despite the failure of previous efforts, such as Rhody Health Options.
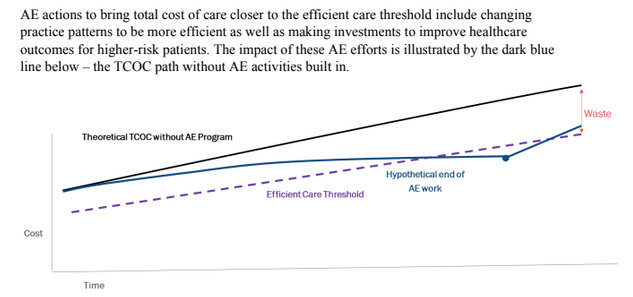
A second feature of the latest version of the Reinvention of Medicaid’s accountable entity initiative is to focus on how best to reduce “low-value care” while investing in care that leads to improved health outcomes, targeting wasteful spending, saying it was aligned with the Rhode Island Foundation’s Long-Term Health Planning Committee’s 10-year plan.
The definition of wasteful spending includes “care that would not have been needed if the patient had received care to prevent and better manage chronic diseases.”
The overarching vision of the Accountable Entity program, as outlined in the introduction to the Year Five plan, states: “Rhode Island’s current system of care does not consistently provide whole-person care, because, as encouraged and reinforced by our fee-for-service (FFS) payment model, it focuses predominantly on medical care of particular health conditions.”
As a result of this model, the report continued “Care is often siloed and/or fragmented rather than coordinated, with high hospital readmissions, avoidable emergency room visits and missed opportunities for intervention.”
Further, although individual providers are performing well, the report said: “No single provider ‘owns’ service integration or is accountable for the overall outcomes of a patient. This makes it more likely that a patient will experience fragmented rather than coordinated care, leading to duplicative services, unsuccessful referrals, and unmet needs.”
The goals of the Accountable Entity five-year roadmap also seemed to focus mostly on cost controls, saying that “Six percent of Medicaid users account for almost two thirds [65 percent] of Medicaid claims expenditures. Disproportionately high expenditures are often associated with populations receiving institutional and residential services.”