Distant thunder on the health care horizon
Escalating costs, consolidation may threaten Rhode Island's plans to reform the health care delivery system
Similarly, the rehabbed 100-year-old Gately Building in Pawtucket, which features 35 rental apartments, will house FarmFreshRI, offering job training and job placement services in the food industry.
PROVIDENCE – It was a busy day at the office, beginning at 7 a.m. on a bright September morning, even before the vigilant meter maid had begun handing out tickets on Point Street. [Birds got to fly, fish got to swim, and the city needs its revenue stream.]
ConvergenceRI held a series of conversations/convergences in the garden oasis that is Olga’s Cup + Saucer with a number of Rhode Island’s more astute health care leaders, including Louis Giancola, president and CEO of South County Health, and Dr. Peter Simon, the recently retired "Dr. Tuesday" from the Providence Community Health Centers.
The topics ranged across a broad landscape of health issues, including the efforts now underway to harmonize metrics around quality and outcomes, driven in part by the State Innovation Model efforts as well as the ongoing workgroup efforts established by Gov. Gina Raimondo to develop a way to cut health care costs in Rhode Island.
In particular, that conversation ventured into how those metrics might need to change to meet the needs of different populations and competing health entities, and where the social determinants of health would fit into the equation as a measurement of community health outcomes – and not just as return on investment for payers and hospital systems in the new accountable care world.
One question that was raised and not answered: Would a one-size-fits-all approach prove to be workable, given that the pieces of the health jigsaw puzzle keep morphing, changing both their shape and colors?
Another focus of discussion was the plans for the toxic stress conversation/convergence scheduled for Wednesday, Oct. 28, at Rhode Island College, in partnership with ConvergenceRI, and the ways that the ongoing initiatives can be brought together as part of a larger conversation, and mapped as an iterative process of health innovation in Rhode Island.
A third topic was about a new report looking at asthma as the leading cause of chronic absenteeism in the nation and the ways in which that was being addressed in Rhode Island, and how the prescriptive data risk analysis now being explored by The Providence Plan might be implemented to identify housing where the conditions that can cause asthma showed the greatest risk.
Neil Steinberg, president and CEO of The Rhode Island Foundation, stopped by briefly to chat on his way to a meeting of his own at Olga’s, offering an observation: who knew that trying to find health care delivery solutions would be so complex?
In turn, Vanessa King, the president and CEO of an emerging Rhode Island-based pharmaceutical development firm also stopped by, promising to call ConvergenceRI in the not-too-distant future to share her firm’s most recent developments.
And, at a nearby table, Megan Hall, former NPR reporter and now a health care consultant, was holding court; one of her newest projects, apparently, is writing a position paper for a statewide health care reform group, HealthRIght.
Juggling costs, conversations and outcomes
It’s no secret that Olga’s often serves as a nodal point as conversations converge in Rhode Island’s health innovation ecosystem.
And, that there are a plethora of ongoing health care discussions, with a lot of balls being juggled in the air at the same time in Rhode Island. They include:
• The working group to reinvent Medicaid has made its final report, and implementation is reported to be underway; the basic premise is still an unproven, a work in progress – that cutting some $180 million in Medicaid costs will result in better outcomes and a decrease in overall health care costs.
• The working group on overdose prevention and recovery is slated to hear the first proposals from its team of public health experts, Traci Green and Dr. Jody Rich, this Wednesday, Sept. 9, on potential interventions.
• The $20 million State Innovation Model [SIM] award continues to develop its plans, percolating mostly under the radar screen.
• A study commissioned by the R.I. General Assembly, overseen by the R.I. Health Care Planning and Accountability Advisory Council and conducted by Truven Health Analytics, will be released in the next two weeks. The study, in four parts, looked at the costs of behavioral health care and substance abuse, building a population health model to evaluate the demand, costs, and supply of services across the lifespan of the recipients served.
• The working group on health care innovation [an odd name choice, more about spin than actual content] is busy wrestling with the best ways to reduce costs from the health care delivery system, exploring the potential to place a cap on costs, similar to what Massachusetts had done. The working group is built upon the statewide compact organized by Steinberg and Sen. Sheldon Whitehouse.
At one of the first working group meetings, David Cutler, an economics professor at Harvard University, who advised Massachusetts legislators in drafting the 2012 law that created the so-called cap on health care expenses in the Bay State, talked about what Massachusetts had done.
Cutler, who had once had Raimondo as a student, spoke about the Massachusetts experience, which he described not as a cap, but a target, according to story in The Providence Journal by reporter Richard Salit. “It’s an overall target on spending; it’s not a cap,” Cutler told the working group.
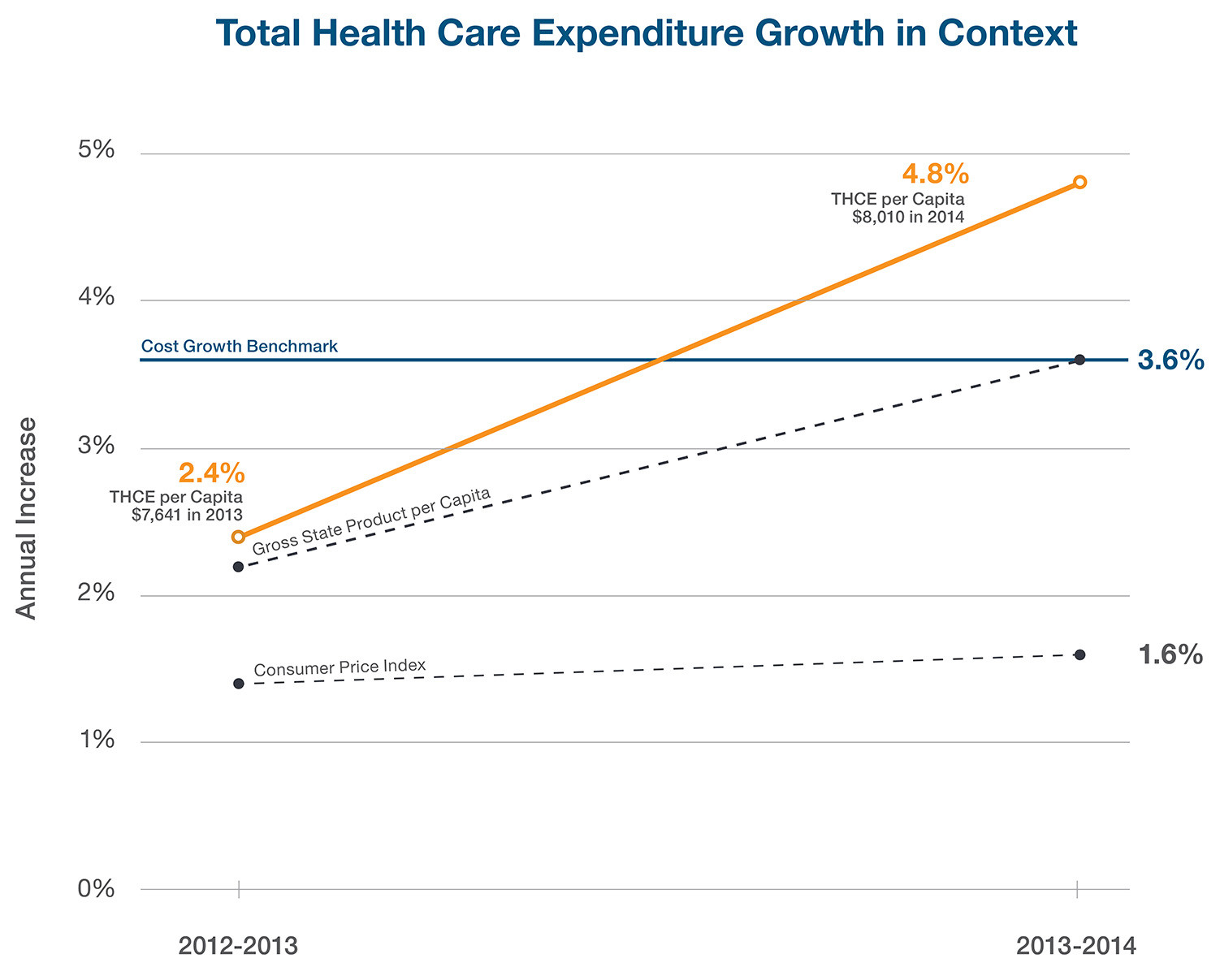
What it does, Cutler continued, is to encourage the health care industry to keep spending under the state’s rate of economic growth, which he said was about 3.6 percent a year. Cutler admitted that there was no legal hammer for exceeding that cap, but rather, in his estimation, there was an opportunity to exert political pressure.
Cutler, who currently serves on the Massachusetts Health Policy Council, said that the state would deliver the message: “If you don’t make it happen, we’ll get very upset.”
Is it now time to get upset?
A new report recently issued by the Massachusetts Center for Health Information and Analysis showed that it might be time for folks to start getting upset in Massachusetts.
In 2014, health care spending in Massachusetts exceeded the 3.6 percent target, reaching $54 billion, a 4.8 increase over 2013 – some $632 million more than the target, according to the report.
The report said that total medical expenses, per member per month, among commercial payers grew by 2.9 percent in 2014, compared to a 1.2 percent increase in 2013 – more than doubling.
It also said that spending for MassHealth, the state’s Medicaid program, increased by $2.4 billion, a jump of 19 percent, while enrollment increased by 23 percent.
The costs shared by members of insurance plans rose by 4.9 percent in 2014, with individual purchasers and small group members continuing to pay the most out of pocket, according to the report.
And the report identified two trends: increased enrollment in high deductible health plans, now 19 percent of the commercial market; and tiered network plans, now 16 percent of the market, appear to show that employers are shifting health care costs to employees.
The report also highlighted a 13 percent rise in drug costs, but Stuart Altman, chair of the board of the Massachusetts Health Policy Commission, acknowledged that there was not much that the State could do to curb drug prices, according to a story by reporter Martha Bebinger.
“There’s much more going on here that we don’t understand,” Altman told Bebinger. “We need to dig deeper to find out.”
Consolidation continues apace
Another big story in Massachusetts with potential big implications for Rhode Island is the announcement last week that Beth Israel Deaconess Medical Center, based in Boston, and Lahey Health, based in Burlington, Mass., are now engaged in merger talks, for the third time.
If the deal goes through, the newly combined health care system entity would create an eight-hospital system, in order to better compete with Partners HealthCare, the dominant health care provider in Eastern Massachusetts, with its 10 hospital-network system, and with the Boston-based Steward Health Care System’s nine hospital-network.
Similarly, in Connecticut, in July, Lawrence + Memorial Hospital of New London, which had recently purchased Westerly Hospital in Rhode Island, announced it has chosen to affiliate with the larger Yale New Haven Health System. The consolidation, according to Bruce Cummings, president and CEO at Lawrence + Memorial, was driven by financial pressures.
How the consolidations to the north and south of Rhode Island will affect the hospital landscape in Rhode Island is unclear: there have been some unconfirmed rumors about a new game of musical chairs around consolidation here.
Distant thunder
It’s not a movie that will ever compete with the numerous Mad Max, Rambo, and Terminator action films, but ConvergenceRI woke up the next morning thinking about Satyajit Ray’s classic, “Distant Thunder,” the tale of how a man-made famine caused by World War II killed more than 5 million people in 1943 in Bengal, India.
The lean, slow-moving narrative, told from the perspective of a young doctor and his wife living in a tranquil village in the Bengali countryside, tells the story of how traditional life was soon overwhelmed by the distant thunder of war.
While there remains an active political debate, even today, about what actually caused the famine, there were many contributing factors: the politics of British colonial control of India [Winston Churchill, in response to an urgent request to release food stocks for India, responded by saying: “If food is so scarce, why hasn’t Gandhi died yet?”]; the religious tensions between Hindu and Muslim populations; and the regional differences that prevented food from other provinces being transported to Bengal.
Here in Rhode Island, amidst the numerous studies and working groups and conversations about how to solve the state’s health care delivery system’s problems, the ever-increasing high costs and disparities in health outcomes, and an intensifying competition between hospital systems to capture a greater market share, there remains a not-so-distant reality that the financial forces of consolidation, operating beyond the state’s borders, may radically change the state’s future health care delivery landscape.
At the same time, there are new initiatives that are gaining traction around the development of health equity, housing and community. As Simon said, heading off to lead a tour of students enrolled in the Brown School of Public Health, “Keep you eye on Central Falls.”