How to map efforts to make Rhode Island a healthier state
Quantifying the risks, illuminating the opportunities, identifying strategies for cost containment – and engaging in a community conversation around health innovation
PROVIDENCE – In health care, we hold most of these truths to be self-evident.
Health care in Rhode Island and America costs too much, and health outcomes, compared to most other countries, are poor or mediocre at best.
The current fee-for-service model of reimbursing care has created perverse incentives. In the long run, it’s an unsustainable system, draining our economy.
All the money spent on health care delivery and health insurance does not necessarily translate into better health outcomes for individuals and communities.
Wasteful spending – on failure of care delivery, care coordination, pricing, over-treatment and administrative complexity – amounts to about one-fifth and one-third of the annual $3.8 trillion spent on health care.
The ability of large systems to change is much like the problems of an aircraft carrier changing direction at sea – it is not nimble. At the same time, any sense of urgency to make the changes often seems lacking.
And, patients, for the most part, have been left out of the conversation.
Mapping a way forward
Where the road divides sharply is over what role government should play in redirecting resources and improving the delivery of health care.
Health care reform and the implementation of the Affordable Care Act have become the nation’s new Antietam and Gettysburg – the battlefields upon which a new national civil war is being waged.
The irony is, as the threat of a spreading Ebola virus confronts the world, no one questions the crucial role that government plays in health care.
The good news is that in Rhode Island, there is an ongoing health care reform evolution now underway – and the train has left the station.
There are a number of pilot programs and initiatives as well as collaborative efforts by insurers, providers and hospitals to cut costs, improve outcomes and involve communities in the process.
There are experiments with the development of Accountable Care Organizations and global payments.
There are new approaches to integration and coordination of care, moving beyond patient-centered to patient-directed care delivery.
There are new health IT approaches that integrate data at the point of care that have successfully bent the medical cost curve; there are also new patient engagement apps that enable patients to track their own health care data.
There are innovative conversation projects about end-of-life care, better integration of hospice and home care, and changes in how seniors are cared for in nursing facilities.
There are proposals to create neighborhood health stations with integrated approaches to the delivery of primary care, through a collaborative network.
There are also statewide programs to create a network of patient-centered medical homes for primary care practices.
There are engaged communities around public health emerging – linking equity to health.
There are new educational programs training nurses to take on the new roles within the patient-centered and patient-directed health care delivery system.
The state’s Office of the Health Insurance Commissioner provides a way to better manage access and affordability of commercial health insurance
There are efforts to connect public health issues – smoking, obesity, lead poisoning, asthma, Hep C, diabetes and heart disease – within a larger behavioral context of prevention and making better choices.
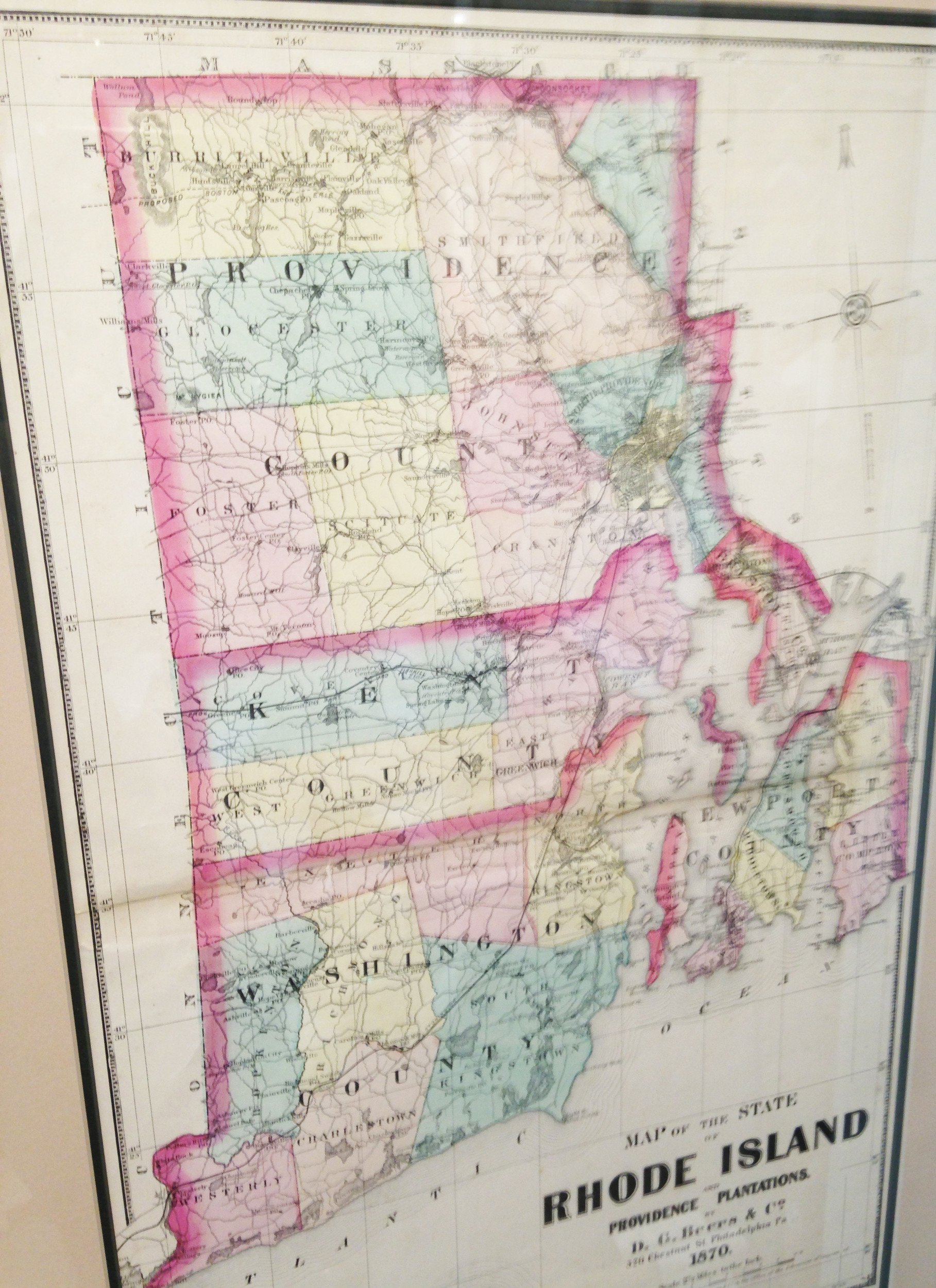
What’s been missing is a way to connect all of these efforts in a comprehensive database and map – one that can be shared across networks and platforms.
The right size
Given the relative small size of Rhode Island and its 1 million population, the state has emerged as an excelling proving ground for such innovative approaches.
The bad news is that there is no mapping of these efforts – and no unified data source tracking the different approaches, leaving consumers and legislators and even hospital systems in the dark about what is actually being done and accomplished.
The worse news is that efforts to develop effective cost containment strategies and a comprehensive statewide health plan have become waylaid by the political divide over health care reform, the expansion of Medicaid and the launch of HealthSourceRI.
The next governor and the 2015 R.I. General Assembly will wrangle about the future of HealthSourceRI and answer the question: should HealthsourceRI stay as a state-run exchange or be absorbed as part of the federal exchange?
But, without a sound, easy-to-understand economic equation that details the costs and benefits and the value of the exchange, and without a better understanding of the role that HealthSourceRI can play in changing the way health care is delivered and costs are contained, the decision will most likely become a litmus test for one’s political ideology. In other words: Are you for it, or against it?
In the meantime, health insurance rates continue to escalate, eating away the both personal and business resources in Rhode Island. The trend of medical utilization rates continues to climb.
As long as the potential, promising solutions are not visible – and not part of any of the political dialogue, the chances for change are diminished.
What would such a map look like?
To create a map of health innovation in Rhode Island, the first task is to create an accurate, inclusive database of the initiatives and pilots now underway.
To do that requires creation of a taxonomy – a way to define and categorize the information, an ordering of the information – as well as an inventory of resources.
It also requires some thought about how to create an online, accessible database, so that the map can be shared and updated as the world of health care changes in Rhode Island.
A third requirement is to make it visually compelling – where the data is more than just numbers but translates easily into evidence-based measurements of results and outcomes.
More than just including the usual “stakeholders,” the mapping process needs to be part of inclusive, public process – iterative in nature, open to input and criticism.
The mapping process, of course, can easily become skewed by political agendas – depending on the funding source. As an example, maps of the new world “discovered” by European explorers tended to project their own worldview. Or, as in the famous New Yorker cover by Steinberg, which depicted New York City as the center of the universe.
A map of health innovation funded by the Hospital Association of Rhode Island would, no doubt, look very different than a map of health innovation prepared by the Rhode Island Health Center Association, representing community health centers.
Similarly, perspectives on mapping health IT innovation would differ greatly between, say, the R.I. Quality Institute and Blackstone Valley Community Health Care.
Perspectives and priorities on health innovation depend on where you are on the health innovation “food chain” – a customer perspective may be different from a health insurer’s perspective or a hospital system’s perspective.
And, a neighborhood health station approach to the integration of primary care and behavioral health may have a different value system than the patient-centered medical home approach developed under an existing group practice, depending on how care is integrated. And, is the priority to reduce risk, to cut costs, or to improve health outcomes? Are hospital systems engines of economic growth or public health?
Differences in attitude
Although the state has embarked on its own pursuit of federal funds to create a State Health Innovation Plan to reform the health care delivery system, the more recent State Innovation Model application reflected the ongoing tension between competing agendas within the state’s health infrastructure.
In one corner of a multi-sided bureaucracy is the state’s Medicaid program, which often walks a political tightrope between lowering its cost within the state budget and efforts to improve the delivery of health care.
The state’s RIte Care program, a successful program to promote health insurance coverage for children and their parents, improving health outcomes and containing costs, has been the target of efforts of state agency administrators and legislators to pare back coverage to parents as a cost-saving measure.
Currently, about 42,000 parents and children are now in the process of being re-certified for eligibility in RIte Care, which has advocates such as Linda Katz from the Economic Progress Institute worried about the numbers of children and parents who may fall through the cracks.
There are also the ongoing efforts, managed by the Rhode Island Medicaid program, known as Rhody Health Options, to create a new unified approach for dually eligible recipients of Medicare and Medicaid.
In another corner is Lt. Gov. Elizabeth H. Roberts and her staff, which created the initial State Health Innovation Plan, hiring the Advisory Board as a consultant, and producing a plan that emphasized the outcome of slowing the annual increase in medical costs to 4 percent from 7 percent over three years.
In a third corner is the R.I. Department of Health, which has moved forcefully in its efforts to invest in improving population health focused on prevention and communities – an approach that is emphasized in the new State Innovation Model application.
In a fourth corner is the R.I. Chronic Care Sustainability Initiative, with ongoing plans to expand the number of practices participating and growing the number of Rhode Islanders seen for primary care in patient-centered medical homes to about 300,000.
In a fifth corner, there are the behavioral and mental health and disability services, advocates and communities – as well as the emerging recovery community.
It’s a complicated landscape, filled with lots of competing agendas for scarce, limited resources. A map of health innovation would visualize the many arms of the bureaucratic Buddha and the intersection with the private sector. It would give added impetus to the need to establish a statewide health planning authority, replacing the current tangled spaghetti-like structure that exists now.
How to get it done?
Health innovation has been left out of the all the current map-making efforts and economic development action plans to date. The question is: who will step forward? The Brown School of Public Health? The Providence Plan? The Rhode Island Foundation? The R.I. General Assembly? The Rhode Island Alliance for Healthy Homes? RIData Hub?
No clear answers seem readily apparent. But, consider this the beginning of a conversation. What do you have to say?