MOU signed with Medicare as part of dually eligible initiative
There is no apparent appetite to discern lessons learned from the launch of Rhody Health Options in 2013, without Medicare
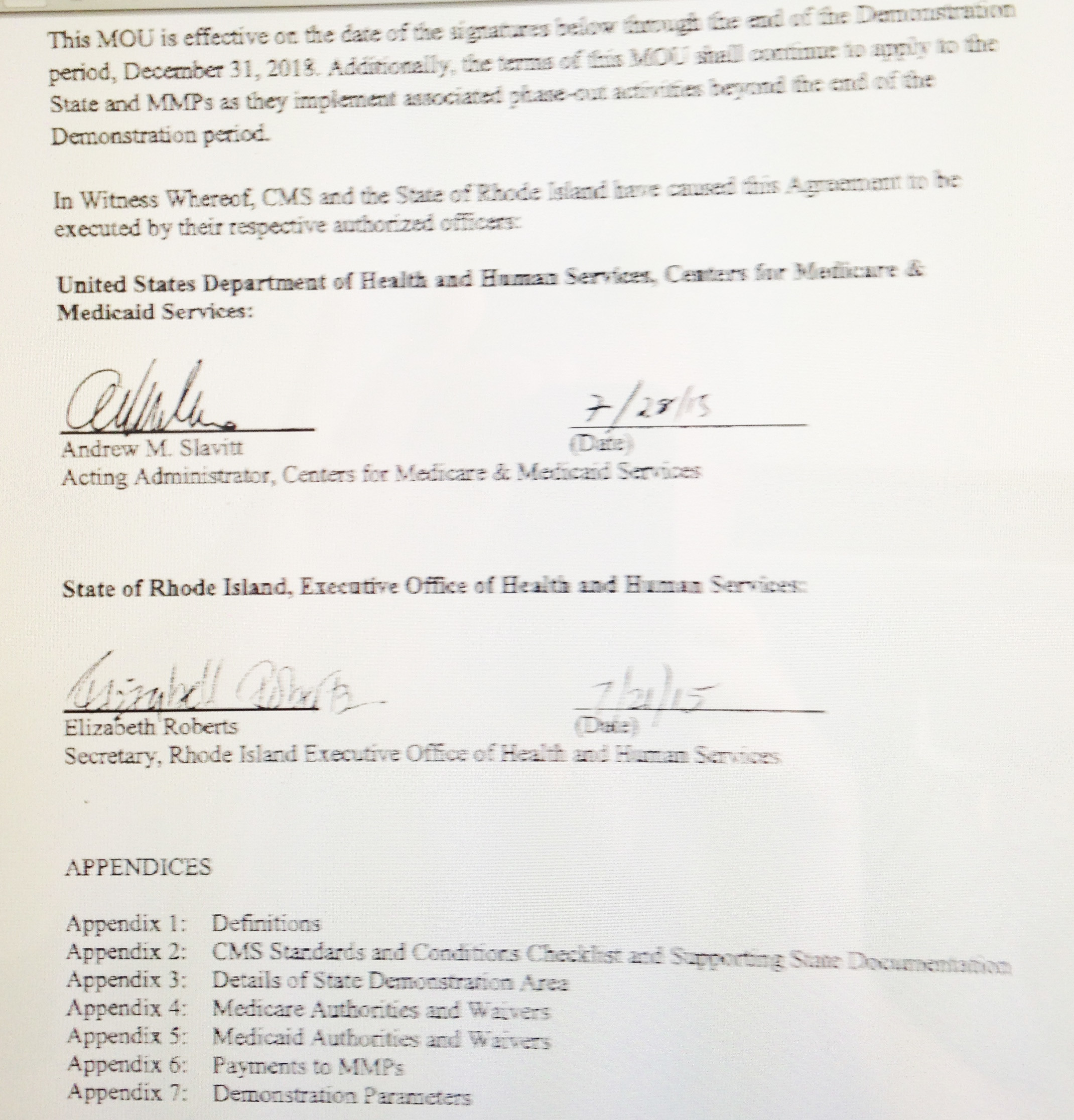
PROVIDENCE – On July 28, Rhode Island became the last of 10 states entering into a capitated duals demonstration project as part of the federal Integrated Care Initiative nationwide to sign a memorandum of understanding with the Centers for Medicare and Medicaid Services,
The 132-page MOU details the conditions for a test of what was called a “capitated financial alignment model” in the delivery of services to dually eligible Rhode Islanders – residents who are eligible for both Medicare and Medicaid.
The MOU spells out in detail financial arrangements for the three-year test of the alignment, set to begin on Dec. 1, 2015, and run through Dec. 31, 2018.
The goal is to reduce the overall health costs driven by this population through better coordinated, better managed care.
The MOU sets the table, finally, for what was always envisioned as a three-legged stool: a contract between the state, CMS, and “one or more” Medicare-Medicaid managed care entities.
The problem has been, up until now in Rhode Island, that the alignment has been skewed: with only Medicaid, through the state, participating, with just one managed care entity, Neighborhood Health Plan of Rhode Island, as the sole source contractor. Without the participation of Medicare and its financial resources, the realignment was much like a pinball machine that always registered tilt.
No accounting for the past
The state of Rhode Island chose to move ahead in 2013 with Rhody Health Options, a plan to bring managed care to Medicaid-covered seniors. Nearly all of these elderly Rhode Islanders had most of their health care services covered by Medicare; Medicaid paid the costs of their long-term care. Without the integration of Medicare, there was no way to coordinate primary, acute and long-term care. Rhody Health Options' added administrative costs were to be covered by the promise of moving some 6 percent of residents in nursing homes back into lower-cost community settings.
Those savings never materialized, and neither did the promised exodus of dually eligible long-term care patients in nursing homes.
At last count, as of May 2015, a total of just 53 dually eligible long-term care patients in nursing homes had been transitioned under Rhody Health Options during the last 18 months.
Few of these 53 transitions were done as a result of Neighborhood Health Plan’s managed care interventions, according to a number of nursing home advocates. They say that most would have happened absent any intervention by Neighborhood Health Plan, through an already exisitng program. Further, there were no metrics or measurements as to whether or not Neighborhood Health Plan had been able to prevent or delay the need for nursing home care among its long-term care enrollees residing in the community.
In terms of managing the money in the contract between Neighborhood Health Plan and the R.I. Executive Office of Health and Human Services, the administrative part of the fees paid to Neighborhood Health Plan ran into the millions last year, for apparently very limited results.
The number-crunching performed under the auspices of the Working Group To Reinvent Medicaid did not delve too deeply into the ongoing financial imbalance at Rhody Health Options and its contract with Neighborhood Health Plan, as best as ConvergenceRI can determine.
For instance, under its risk-sharing agreement with the state, Neighborhood Health Plan claimed $9.5 million, to cover its losses in 2014.
At the center of the policy assumption in the working group’s proposed reinvention of Medicaid is that creating a community-based system of care instead of investing in long-term care in nursing facilities will create cost savings and improve care.
It is also a central component of the assumptions behind the Integrated Care Initiative and the realignment of Medicare and Medicaid spending on the dually eligible population.
But, what hasn’t been calculated yet is what the actual costs will be of creating a comprehensive community-based system of care. It may turn out, despite the best of intentions, to be a prohibitively expensive health care delivery system.
The biggest factor arguing against the success of the comprehensive community-based system of care – as currently defined in the Integrated Care Initiative – is Rhode Island’s demographics. As commentator Scott MacKay from Rhode Island Public Radio phrased it: “We have one of the highest populations of fragile elderly in the country. What’s happening is, folks have Alzheimer’s, they have dementia; it’s very expensive to care for these people. How do we deal with these kinds of illnesses that require institutionalization?”
Back to the future
Now that the MOU with Medicare has been signed, and with it, the third leg of the stool has been secured in the realignment of payments for dually eligible Rhode Islanders, many are optimistic about the opportunities to rebalance the system of care delivery.
It’s clear that no one in state government has any appetite to discern any lessons learned from the rollout of Rhody Health Options in 2013; the poor financial performance of the initiative will apparently be swept under the rug, with no accountability.
Under the new MOU, Medicare sets out some very detailed financial and quality metrics and standards to be achieved. These include reductions in payments to be achieved: 1 percent in the first year; 1.25 percent in the second year, and 3.3 percent in the third year.
Another fascinating part of the MOU is the language around contracting with “one or more” managed care providers. The language in the news release issued by CMS that announcing the new MOU was called “coy” by one local health care expert, as it related to future contracts with managed care providers.
The question is whether or not Neighborhood Health Plan will continue as a sole source provider under the new arrangement. CharterCARE’s parent, Prospect Medical, has indicated its interest in obtaining a share of the managed Medicaid population. Medicare is where the money is, when it comes to dollars spent on health care delivery for dually eligible persons.