Primary care evolution in Rhode Island prepares for next leap forward
Taking notes at the 2014 annual Learning Collaborative for CSI-RI
WARWICK – What started as a pilot project with five primary care practices six years ago in 2008 has now evolved into a “movement,” according to Dr. Thomas Bledsoe.
The movement is the Rhode Island Chronic Care Sustainability Initiative, or CSI-RI, which now encompasses 36 primary care practices that provide health care in patient-centered medical homes to some 200,000 Rhode Islanders – and with plans underway to add 20 more practices serving an additional 100,000 adults, one-third of the state’s population.
That was one of the messages that Bledsoe, co-chair of CSI-RI Executive Committee and an internist at University Medicine, delivered to more than 200 participants who had gathered for the 2014-CSI-RI Annual Learning Collaborative, “The primary care team: the future is now,” at the Radisson Hotel on Oct. 9.
The initiative, an all-payer collaboration of commercial insurers and Medicare and Medicaid, was begun under the leadership of former R.I. Health Insurance Commissioner Christopher F. Koller. Today, the fiduciary agent is The Rhode Island Foundation, and its efforts are funded through an affordability standard established by the R.I. Office of the Health Insurance Commission in 2010 under Koller.
Bledsoe recalled that CSI-RI’s first learning collaborative had been held in the same room, with about 20-30 people attending. “If you look around, you can see what we’ve done over the course of last six to eight years,” he said. Think back, he continued, about what your practice was like and what the patients were like. “What we have is a collaborative process that the rest of the country looks at with envy.”
The half-day Learning Collaborative marked a number of transitions for CSI-RI – including a new name. Moving forward, it will known as Care Transformation Collaborative, with a website branded as PCMH Rhode Island.
In addition, the gathering considered a number of new primary care initiatives: end-of-life care, patient-engagement technology, online weight loss programs, models to better integrate behavioral health, pain in pediatric primary care, and community health teams.
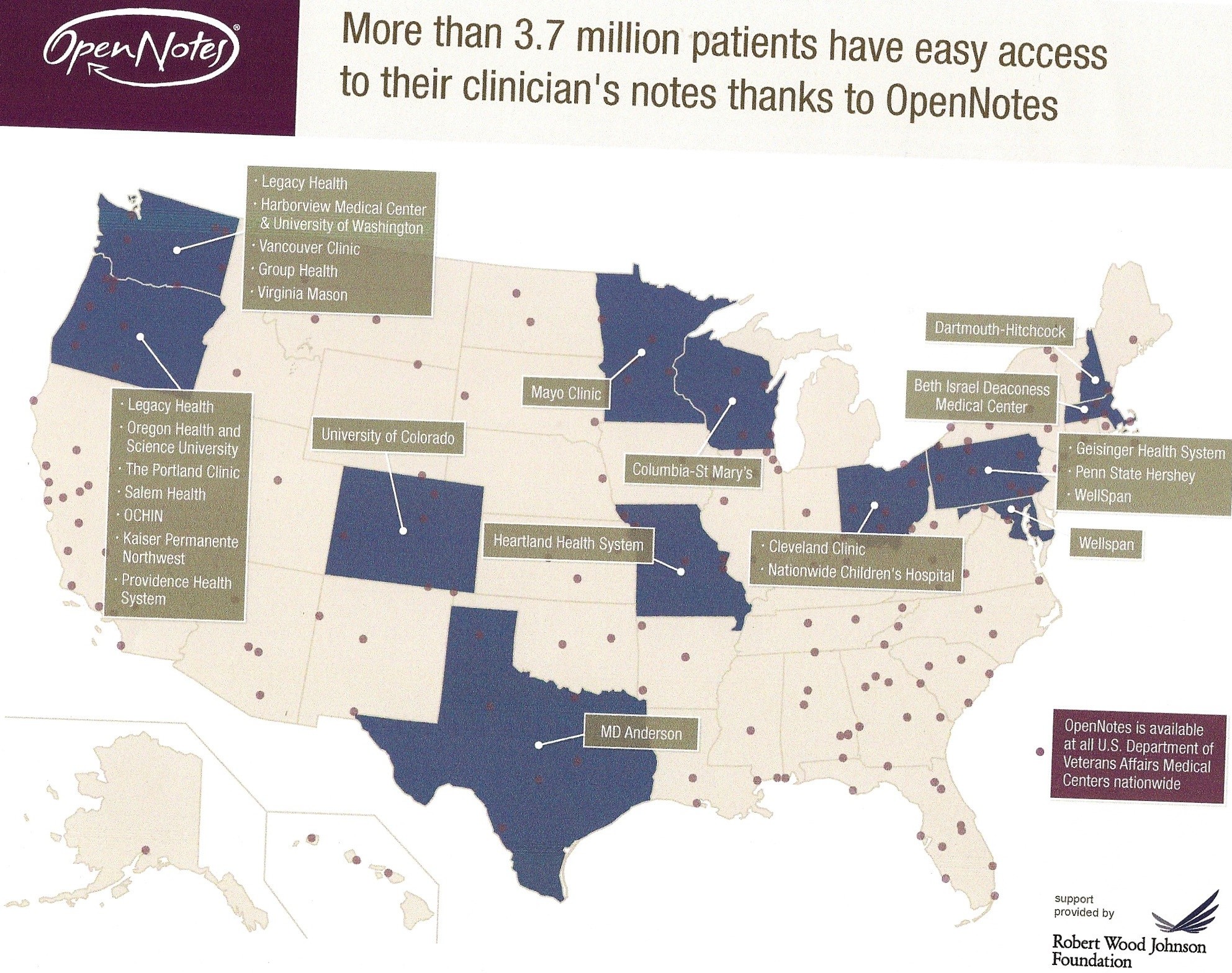
One of the more proselytizing presentations was by Jan Walker from Beth Israel Deaconess Medical Center, who urged the patient-centered medical homes to adopt OpenNotes, a transparent process of sharing providers’ notes with patients that has also become a movement, with 3.7 million patients now having easier access to their clinicians’ notes.
But there was also some important news buried in the opening remarks by Dr. Kathleen Hittner, the current R.I. Health Insurance Commissioner, that the annual 1 percent charge on the medical spend to support primary care is being phased out.
Hittner’s news
Hittner began by paraphrasing an old C&W standard, “I was country before country was cool,” by saying that those who began the CSI-RI initiative had known that primary care was sexy before everyone else had.
Hittner gave the audience a broad overview of the four affordability standards, focusing first on the 1 percent annual increase, saying that primary care spending had reached a total of about 10 percent of the overall medical spend – a $64 million increase. As a result, she said, that while OHIC will “continue to support primary care, we’re not going to it with a 1 percent per year increase, because we’re over 10 percent of the spend.”
Instead, she explained that OHIC was going to do a study of how the state’s medical spend on primary care correlated with the rest of the country.
In addition, Hittner pledged that OHIC was going to redouble its efforts to support CurrentCare, also one of the targets of the affordability standards.
“We are definitely supporting CurrentCare,” she said. “This is a pivotal year for CurrentCare,” although she didn’t explain exactly why that was so. “There are over 400,000 patients now enrolled,” she continued, and playing the role of cheerleader, she said: “We have to make it so everyone one of you goes to CurrentCare to look up the things you need to see what’s happening with patients, to avoid unnecessary testing and things of this nature.”
Hittner asked the audience how many were members of CurrentCare, and only about one-fifth raised their hands.
Hittner ended by assuring the audience that even though the affordability standards were going to be continued in “a little different way,” her office will continue to support CSI-RI and its growth.
A message from Neil Steinberg
Neil Steinberg, the president and CEO of The Rhode Island Foundation, opened the session by thanking every one, acknowledging “the converging” of so many people as a result of CSI-RI.
Steinberg praised the initiative, saying it was one of the top initiatives The Rhode Island Foundation was involved with, focused on “affordability, accessibility of primary care, so that everyone who wants it and needs it should have it.”
We pleased and proud, Steinberg continued, “to support an innovative model of primary care that takes a team-based approach. We look very smart for having supported it.”
Steinberg closed by providing an economic development context to the work of CSI-RI: “If we can say we have the best primary care and the best public education in the United States, we will not have to do anything else for economic development, because folks from all over the country will flock here to Rhode Island.”
OpenNotes
The presentation on OpenNotes by Walker offered compelling research and patient stories to back up her pitch.
After a year’s trial in three different settings – Beth Israel Deaconess in Boston, a rural community in Pennsylvania served by Geisinger Health System, and Harborview Medical Center in Seattle, Wash., a safety net hospital that served many homeless patients – 99 percent of the patients wanted to continue receiving e-mails of their clinical notes. Only 75 percent of the clinicians said they wanted to continue, but faced with the overwhelming desire of the patients to continue, the 25 percent who had wanted to leave opted to stay with the program.
Walker defined OpenNotes as “visit notes written by clinicians that the patients can access on line through secure portals.”
She cited research that showed patients often forget what they hear during a visit to a doctor’s office, because of the intensity of the visit, even if nothing is wrong.
The concept for OpenNotes originated with the idea: what if we made those notes about the visit available to patients to refresh their memories. Could we get patients to look at the notes online, either on a computer or a mobile device? Would patients become more engaged? Would it improve the clinician-patient relationship? Would patients become a better team member?
The use of OpenNotes, similar to CSI-RI in Rhode Island, has become an emerging movement. OpenNotes is available at all U.S. Department of Veteran Affairs Medical Centers Nationwide.
Walker also said that some of the initial concerns voiced by clinicians – that the patients wouldn’t understand the notes or would be too worried by what was said – proved not to materialize in the practice of sharing notes. It also did not appear to increase the work load of the clinicians, though many said that they now took more care in writing notes.
Currently, there are no patient-centered medical homes in Rhode Island that are using OpenNotes, but that may be changing shortly.