The new geometry of governing
A wave of corporate consultants has become the hallmark of the way that Rhode Island now makes policy decisions and governs
PROVIDENCE – Four major news stories broke during the first full week in July, with most of Rhode Island still on vacation, including ConvergenceRI. [No, the stories didn’t include the unexplained explosion on the beach in Narragansett, which sent the news media into a tizzy; nor did they involve Donald Trump.]
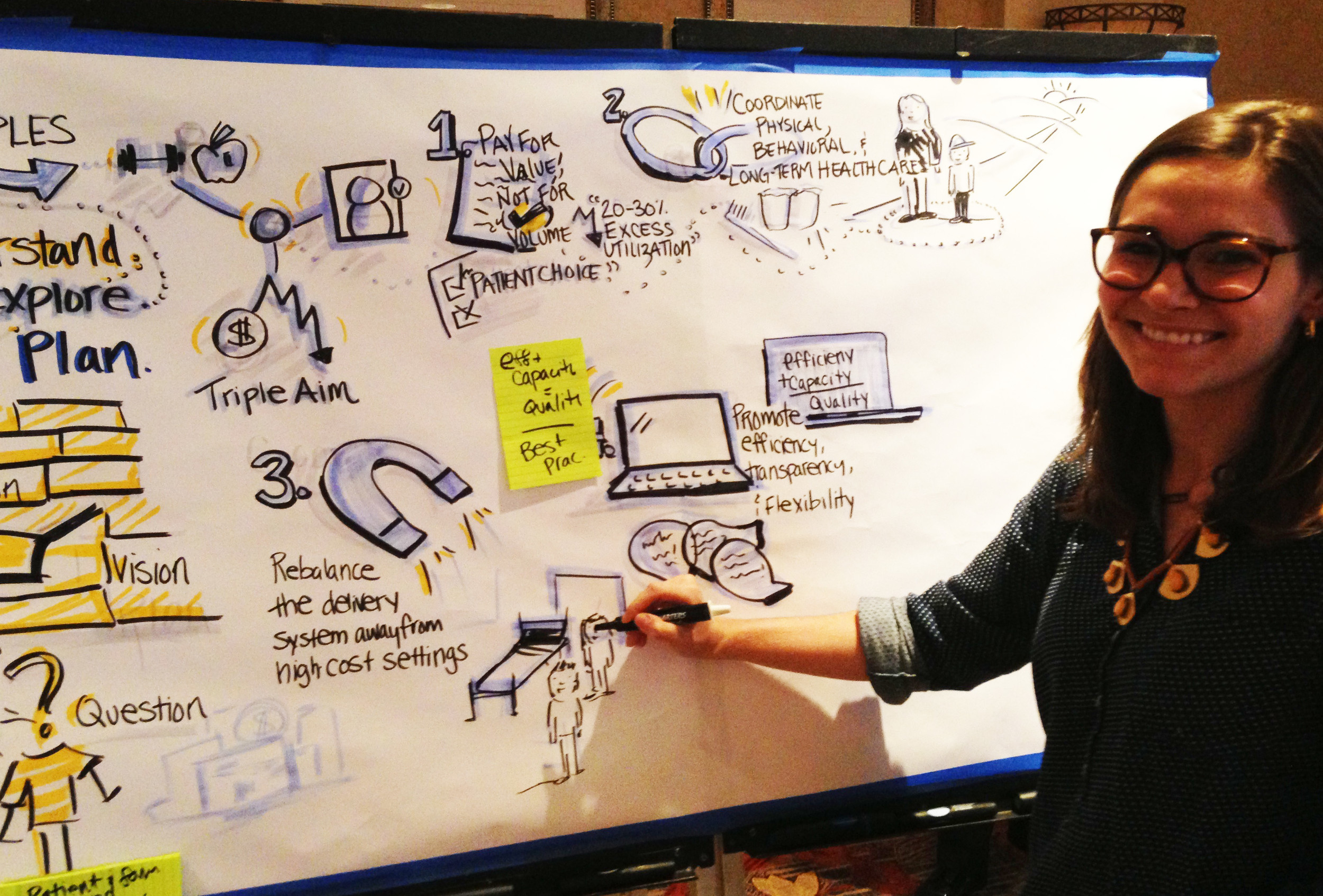
In case you missed it: a final report on reinventing Medicaid in Rhode Island was issued on July 8; the appointment of Rhode Island’s new education commissioner was also announced that same day. The day before, on July 7, a new executive order was signed to create a new working group to cut costs through a reinvention of Rhode Island’s criminal justice system; and, on July 8, a hearing was held on a new state planning report on affordable housing in Rhode Island.
Call it synchronicity, serendipity, or carefully managed public relations: the resulting news coverage produced stories that could best be described as silos on steroids. [At least that’s the way it appeared to ConvergenceRI, upon re-entry into Rhode Island’s murky atmosphere, after five days in Vermont.]
Few would argue against the fact that, at their roots, state policies on housing, prisons, health care delivery and education need to be intimately interconnected to each other [albeit, in a different fashion than the current web of convoluted, unhealthy, co-dependent relationships].
Yet, all of the policy changes, initiatives and analyses announced during the second full week of July were dealt with as separate streams of policies, information and news – silos that never seemed to converge, serving as a kind of 21st-century proof of Euclid’s parallel postulate, as if the Earth was flat.
The disconnect in the news coverage reflected, very accurately, the silos that exist between state policies on housing, prisons, health care delivery and education, in spite of the current wave of reinvention.
Investing in policy without evidence-based results and benchmarks leads to a kind of magical thinking, driven by ideology, where policies are developed and implemented, without knowing whether or not they actually will work.
“Whatever the reality is, they will tell you it’s a success,” said one leading advocate of health care reform in nursing homes and assisted living, criticizing the absence of metrics in the newly released plans to reinvent Medicaid. In Medicare, by comparison, she continued, there are some 18 different quality measurements to benchmark performance.
Indeed, the advocate pointed out, Gary Alexander, the former head of the R.I. Executive Office of Health and Human Services, was still getting paid six figures as a consultant, including $220,000 by the state of Arkansas and $925,000 by the state of Maine. The Alexander Group on its website still touted the alleged success of Rhode Island’s global Medicaid waiver from 2009, claiming Alexander achieved a $100 million in savings through “rebalancing” the state’s Medicaid costs – which was never achieved.
To cross that big river denial
Politics is still the story about who gets want, when, and for how much.
Government policies around housing, education, health care and prisons are as much about the flow of money as they are about the flow of ideas.
What follows is an ambitious three-part story; it attempts to reframe Rhode Island’s governing landscape by breaking down the silos and by identifying points of convergence. In doing so, the aim is to begin the conversation around a new kind of holistic mapping of innovation in Rhode Island, and to identify the many rivers that need to be crossed. [It was, truthfully, too big and unwieldy to write as one story.]
It begins with a philosophical launch, asking questions about the gaps in policy. It ends with questions about the wave of corporate consultants that have become the hallmark of the way that Rhode Island now makes policy decisions – and governs.
The biggest river to cross, of course, is denial – the kind of magical thinking that says the reinvented policy designs will be successful, without first testing them with any evidence-based metrics. What if they fail?
And, the belief that cost-cutting strategies, without increased investments in capacity, resources and infrastructure, will lead to a greater return-on-investment on government spending. Will reduced spending on nursing homes ever trump Rhode Island’s demographics of having more older, frailer seniors in need of 24-hour care?
PART 1
Question: How can you begin to figure out how to achieve better health and educational outcomes without talking about the lack of affordable, healthy housing?
Housing, Elizabeth Burke Bryant, the executive director of Rhode Island Kids Count, told ConvergenceRI, “is the ultimate children’s issue, where children are able to rest their heads at night.”
Too many Rhode Island children are living in homes where there is a high cost burden, Bryant continued, speaking in advance of a new national report that will be issued on Tuesday, July 21, by the Annie E. Casey Foundation.
Bryant, who recently sat down to talk with Betsy Stubblefield Loucks of the R.I. Alliance for Healthy Homes to develop common ground around a shared healthy housing agenda, said that the relationship between housing, health and education was central to the well-being of children in Rhode Island.
“No issue shows that more than childhood lead poisoning,” she said. Yet, despite the steady progress being made, Bryant continued, “There are continuing pockets of lead poisoning in some of our core cities.”
Lead poisoning, Bryant said, “is a preventable, serious pediatric health condition,” resulting in a greater risk of special education, compromising children’s brains and brain functions, impacting educational outcomes.
“It’s a completely preventable issue,” Bryant said, her voice rising in anger.
Sen. Jack Reed, on June 25, called lead poisoning a curse that afflicts low-income, older neighborhoods. “Once a child is infected by lead, that child’s cognitive ability, that child’s ability to succeed in school and to contribute to this community, is devastated. And, it’s completely avoidable. You simply have to get the lead out.”
Errors of omission
Question: Why, then, are policies on how to reduce and eliminate the scourge of lead poisoning in Rhode Island missing from policy reinvention discussions on health, education and prisons?
The facts are damning: lead poisoning is a long-term, lifetime threat to a Rhode Island child’s future educational and economic attainment [and a suspected contributing factor in the risk of incarceration].
The research shows that elevated levels of lead have a prolonged and deleterious effects – in testing scores, in school readiness, in reading capability, in higher costs for special education interventions, and in school suspensions in continued behavioral problems. Those effects do not fade over time, but increase, as children become adults, according to researchers.
As James Heckman, Nobel laureate in economics, explained it, you can predict the future number of prison beds needed by the number of students who cannot achieve fourth-grade reading levels.
The persistence of lead poisoning in Rhode Island, despite the progress made in screening children and the increase in certifying homes to be lead-free or lead-safe, continues to play out in the significant loss of human capital, according to Anna Aizer, associate professor of Economics at Brown University at The Population Studies and Training Center.
Since 2004, the gap between white and black children has remained a constant in Rhode Island, with blacks at higher risk, according to Aizer. New research is underway to look at crime data and outcomes with respect to criminal behavior and lead exposure, according to Aizer.
Removing lead in homes is a cost-effective solution. The return on investment for removing lead is calculated to be $220 for every $1 invested, according to Ruth Ann Norton, president and CEO of the Green & Healthy Homes Initiative, based in Baltimore, Md.
But, in the final report of the working group to reinvent Medicaid in Rhode Island, there is no mention of lead poisoning or programs to invest in the removal of lead from housing.
There is only, first, an acknowledgement that there are challenges that Medicaid is not fully equipped to address: “The population served by the Medicaid program often faces challenges associated with social factors such as housing [emphasis added], food insecurity, and health literacy; challenges the current system is not fully equipped to address.”
And secondly, the acknowledgement that social determinants of health are not usually covered by health insurance: “[The] inability to address social determinants of health that are not typically covered by health insurance: lack of food, clothing, employment, or shelter [emphasis added] can make it impossible for healthcare interventions to be successful, resulting in ineffective use of high cost interventions when lower cost provision of these basic needs could result in improved health.
On a more positive note, the report, without details, encourages a broader focus on non-medical interventions, but without any specific source of resources: “Medicaid must support – and fund, where possible – a wider focus on non-medical interventions and social determinants that, if resolved, can often reduce utilization, lower costs and encourage healthier lifestyles.”
In the data-driven research planned for Rhode Island’s criminal justice system to promote cost-cutting solutions, there are no plans to ask or answer any questions, or to mine existing data, or to cross-reference ongoing research to identify lead poisoning among those incarcerated, according to the consultants responsible for producing the study.
Much of the initial conversations with Ken Wagner, the new commissioner of education in Rhode Island, have focused on curriculum, standardized testing, teaching evaluations, the role of charter schools. Lead poisoning has not been part of the conversation.
Errors of commission
Question: How can you come up with a cost equation to achieve better health outcomes without addressing health equity and the social determinants of health, in relationship to economic disparities around housing and education?
Beyond the omission in policy discussions about the deleterious effects of lead, which is an equal opportunity offender, cutting across the housing, education, health care and prisons sectors, there is a need to acknowledge the reasons behind the lack of investment in many neighborhoods: racism and greed.
That’s the message that Dr. Mindy Thompson Fullilove, a professor of Clinical Psychiatry at Columbia University, in her discussion of urban renewal in America in the 20th century. “Health equity was swept away by racism and greed,” Fullilove said at the Rhode Island 2015 Health Equity Summit in May.
Fullilove dissected what happened in cities such as Pittsburgh and Cleveland through redlining of the cities by banks, driving diversity out of the urban centers, pushing black families into increasing crowded neighborhoods that were outside the zone of new investment.
Fullilove’s conclusions were echoed in the recent state planning report on affordable housing in Rhode Island.
“Almost 70 percent of Rhode Island’s black and Latino communities live in three communities – Providence, Pawtucket and Central Falls, all with school systems that face significant challenges not encountered in most of the state’s suburban school systems,” as reporter Christine Dunn wrote in her story in the Providence Journal, citing the findings of the new state planning document. Why is that? Did it happen by accident or design?
As the Minority Health Facts 2015, published by the R.I. Department of Health, state unequivocally: “Rhode Island’s racial and ethnic minority populations often feel the burden” of the social determinants of health, resulting in health disparities. At best, only about 20 percent [some say the number is closer to 5 percent] of the money spent on the health care delivery system is spent on health, wellness and prevention. How does the development of community-based health equity zones, or the development of neighborhood health stations, fit into the reinvention formula? Why are such alternatives not part of the conversation? And, how does the community participate in the decision-making around health investments?
Errors of avoidance
Question: How can you attempt to reinvent the state’s criminal justice system without addressing the crisis in addiction, where statistics show that some 63 percent of Rhode Islanders that are in jails, on parole or probation because of issues related to substance use and abuse?
The reinvention of Medicaid group published its report, and, right on cue, another working group of stakeholders begins its task of reinventing the criminal justice system. Two executive orders, two parallel lines that do not appear to intersect or overlap, two silos.
“No one from the criminal justice system ever presented numbers or participated in the working group conversations,” said Holly Cekala, a member of the Medicaid working group, when asked about the silos by ConvergenceRI.
“No one [from the criminal justice system] ever came to talk about the pseudo-state hospital that is our prison system,” Cekala continued. Or, “Why 78 percent of the so-called Medicaid ‘super-users’ [targeted for cost-reduction strategies in the plan] had a prison history.
While Cekala praised the worthy goals of the working group, she questioned the state’s capacity to implement the changes.
The failure by the R.I. General Assembly to re-enact the Good Samaritan Law reflects a fundamental policy disagreement between R.I. Attorney General Peter Kilmartin and many public health leaders about whether addiction should be treated like any other chronic illness. Is an overdose a medical emergency or a crime scene?
Does Kilmartin believe that Rhode Island is going to arrest or incarcerate its way out of this crisis? You can’t reinvent the criminal justice system in Rhode Island until there is a public debate and resolution of this contentious policy divide.
Further, unless you can create evidence-based research that identifies family violence and sexual abuse [in addition to lead poisoning and toxic stress], not just as causative factors, but tracks policy interventions about what works and what doesn’t work, the metrics for success are missing.