New OHIC report recommends $45M increase in Medicaid provider rates
Report provides a destination but not a roadmap
The Attorney General continued: “Our actions and your coverage of our actions can help to inform the public about these rising costs and the way they can have their voices heard. In addition, the process would be more robust with greater input from people ‘on the ground’ who are experiencing the effects of unaffordable insurance, engagement that could be accomplished with outreach.”
AG Neronha concluded: These OHIC proceedings occur every year and the timeline is very similar from year-to-year, so we encourage you and all members of the public to watch the OHIC website if you want to participate.”
PROVIDENCE – The 50-page report, the “Social and Human Services Programs Review,” produced by the Office of the Health Insurance Commissioner under the direction of Acting Health Insurance Commissioner Cory King and delivered on Friday, Sept. 1, to Gov. Dan McKee, House Speaker Joseph Shekarchi and Senate President Dominick Ruggerio, does not pull any punches.
The report recommends a $45 million increase [emphasis added] in Medicaid provider fee-for-service rates in the next fiscal year, focused on three major areas: behavioral health [including substance use treatment], children’s services, and home and community-based services.
The OHIC recommendations for Medicaid rate increases, the report says, “represent a destination [emphasis added] for reimbursement rates, but do not furnish a road map [emphasis added] for getting there.”
Still, the report continued: “The proposition of investing in our health care system through the mechanism of Medicaid reimbursement rates is an attractive one because state investments in Medicaid will leverage new federal dollars for Rhode Island’s economy and help to support its health and human services workforce.”
After years of apparent unwillingness by the General Assembly to invest in paying Medicaid providers, the new OHIC report provides a detailed breakdown and rate review strategy on how best to move forward. The question is: Will the report create enough of a political groundswell to push legislators and the Governor to take action?
The first task, of course, will be for people to read the densely written report. [See link below to the report.] Then it will be incumbent upon community agencies and advocates to champion the report’s recommendations as part of their legislative agenda. For instance, how will Rhode Island Kids Count incorporate the report’s finding into its upcoming legislative policy agenda?
OHIC will be hosting a public forum in two weeks, on Friday morning, Sept. 22, beginning at 10 a.m. in Conference Room 2A of the Department of Administration building, to provide the general public, stakeholders, providers, and Medicaid recipients to provide comments and ask questions.
Quantifying the need
The report provides a detailed analysis as well as recommendations for how to conduct future Medicaid rate reviews – the kind of analysis and benchmarking and methodology that has often been missing from the discussion around the delivery of health care services in Rhode Island.
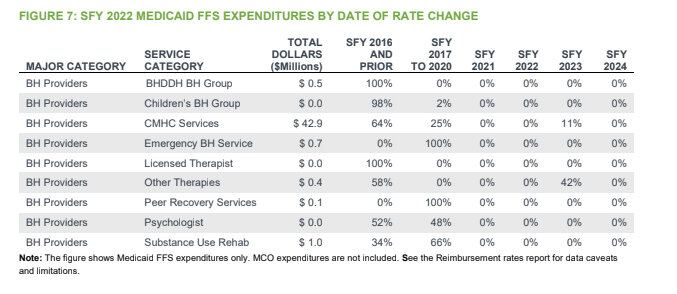
For instance, the need to increase Medicaid rates for providers was made perfectly clear in Figure 7 in the report, which provided a detailed, comprehensive analysis of the Medicaid Fee-For-Service rates by the date of rate changes for behavioral health providers. [See image above.]
Translated, the documented lack of rate increases [emphasis added] for the state funding years from 2017 through 2024 for Medicaid behavioral health service providers shows what appears to be systemic neglect, in ConvergenceRI’s opinion.
The report also provides valuable comparisons between Medicare rates for behavioral health services, finding that “Medicare reimburses at approximately 130 percent to 300 percent of the Medicaid FFS rate.”
Further, the report found: “On average, Medicaid MCOs pay approximately 106 percent of the Medicaid FFS rate for benchmarked services. “Given the relative consistency between Medicaid FFS and MCO reimbursement levels, it is possible that a portion of Medicaid MCO services are established as a function of Medicaid FFS reimbursement,” the report said, adding: “This last finding is important. To the extent that Medicaid MCO reimbursement rates are established as a function of the Medicaid fee schedule, changes in the Medicaid fee schedule are likely to generate changes in the reimbursement rates paid by MCOs to their contracted providers.”
Details, details, details
For readers looking for the specifics of the rate recommendations, the analysis can be found in Section 5 of the report, where it “describes the rate recommendations in great detail and presents composite recommended rate adjustments and rate adjustment ranges for each major service category.”
Further, Appendix 1 “provides recommended reimbursement rate adjustments for each specific service code. These recommendations are based on analysis of economic data and program access.”
Context and nuance
The new OHIC report and its recommendations to increase Medicaid provider reimbursements come at a time when there is increasing turmoil in the health care delivery system in Rhode Island. Primary care is in crisis; the health care workforce is in crisis; hospitals are struggling to keep their financial operations afloat; the future of two hospitals, Rogers Williams Medical Center and Our Lady of Fatima, owned by a for-profit private equity firm, Prospect Medical Holdings, are in danger of closing; and the mix between private and public payers has made it difficult for hospital systems in the state to maintain their financial sustainability. Stay tuned.
Editor’s Note: In the coming weeks, ConvergenceRI will undertake a more comprehensive analysis of the OHIC report, including interviews with Acting OHIC Commissioner Cory King and numerous other stakeholders.