The latest salvos between Lifespan, Care New England
Public hearing on Certificates of Need for obstetric facilities offers a preview of the latest battle in the struggle over who will control the women’s health market in Rhode Island
The integration of the work being done by Keating and by Barry Lester needs to become a component of the overall approach to maternal and child health.
PROVIDENCE – Of all the decisions to be made by Dr. Nicole Alexander-Scott, the director of the R.I. Department of Health, that will shape the future landscape of health care in Rhode Island, perhaps none will be more significant than the outcome of two pending applications for certificates of need for obstetric facilities, one by Lifespan, the other by Care New England.
Rhode Island Hospital, the flagship of Lifespan’s health system, has proposed building a new obstetrics facility on two floors atop Hasbro Children’s Hospital, with 31 beds, at a cost of $43.2 million to construct and a projected $18.6 million a year to operate. If approved, construction would be finished in 2020, with the capability of handling some 1,600 births per year, according to Lifespan.
The new obstetrics facility would be a mere few hundred yards away from Women & Infants Hospital, the flagship of Care New England’s health system, at which some 8,900 babies were delivered in 2016, more than three-quarters of all births in Rhode Island.
Care New England, in turn, has proposed renovating its existing Birth Center at Women & Infants Hospital at a cost of $18.6 million, with a scheduled completion date of October of 2018, with half of that money to be raised through philanthropy. The goal is to renovate the 30-year-old facility to create an intimate care environment that matches the clinical excellence of the hospital.
As Dave Duncan, vice president of Facilities at Care New England, asked rhetorically during his recent public testimony in support of the planned renovation at Care New England: “What was the car like that you were driving 30 years ago? And, would it meet your needs today?”
Squaring off
At a public hearing held on May 2 by the R.I. Health Services Council in the basement of the R.I. Department of Health, the two sides squared off, with more than 100 in attendance. Most of the public testimony came from representatives of Care New England, often in emotional, passionate voices, opposing the Rhode Island Hospital proposal and promoting the Women & Infants renovation proposal.
Testimony from Lifespan came from Jodi Bourque, Associate General Counsel for Lifespan, who previously worked on health care issues for the R.I. Attorney General’s office. She shared key points from a three-page letter submitted to Michael Dexter at the R.I. Department of Health.
Though the two Certificate of Need proposals are separate, they are inextricably linked by the ongoing conflict between the two largest health systems in Rhode Island.
What is at stake?
Alexander-Scott has been put in the Solomon-like position of having to decide which health system will have “ownership” of the delivery system for babies in Rhode Island – as well as capture the future market share for women’s health care in the state.
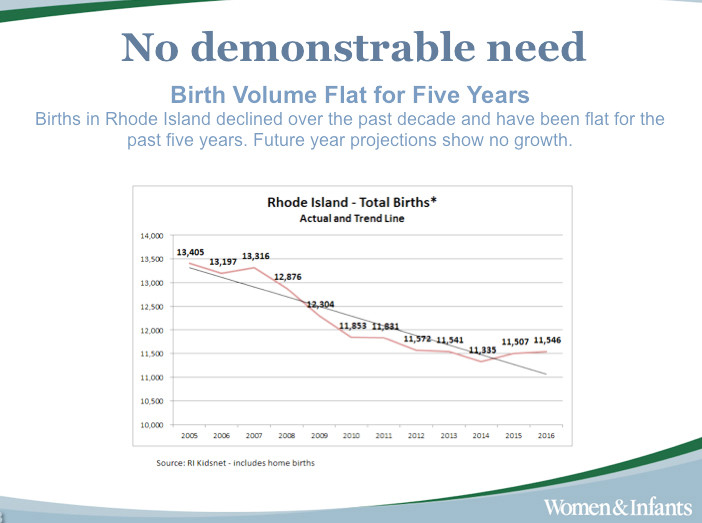
An overarching question is this: with the number of births in Rhode Island having declined over the last decade, and the actual birthrate having been flat for the past five years, with 11,831 in 2011 and 11,546 in 2016, is there a demonstrable need for such a new obstetrics facility?
Further, with projected demographics showing an aging female population in Rhode Island projected through 2021, what is the likelihood that the demand for birthing services may further decline?
While not objecting, per se, to Care New England’s proposed renovation, Lifespan’s Bourque raised questions about the significant financial difficulties encountered by the Care New England health system and how its potential relationship with Partners Healthcare in Boston might change the equation.
[It should not be lost on any members of the R.I. Health Services Council that Lifespan was not happy that Care New England spurned Lifespan’s bid to merge in the most recent round of musical chairs of consolidation, instead choosing Partners.]
At a time when state funding resources are constrained, when the federal health care policies and funding are being disrupted with the repeal and dismantling of the Affordable Care Act underway in Congress, it promises to be a time of heightened concern.
All the big issues swirling about health care in Rhode Island – medical cost control, quality of care, competition, consolidation, market share, insurance coverage, population health and health equity – will come into play in making the decisions.
Historical context
The latest conflict between Lifespan and Care New England over control of the women’s health market has it roots in a move by Lifespan to bring a number of former providers at Women & Infants under its corporate wing six years ago.
In 2011, Lifespan created the Women’s Medicine Collaborative, an outpatient medical group of women providers, many of whom had previously worked at Women & Infants Hospital. The co-founder was Dr. Karen Rosene-Montella, who then became Lifespan’s senior vice president for women’s services and clinical integration.
In 2013, Lifespan partnered with Ob-Gyn Associates, Inc., one of the largest obstetrics and gynecology practices in Rhode Island, integrating them within services offered through the Women’s Medicine Collaborative.
In 2016, Lifespan first announced plans to build its own new obstetrics unit on the Rhode Island Hospital campus.
Mark Montella, senior vice president of External Affairs at Lifespan [and the husband of Dr. Karen Rosene-Montella] described the thinking behind the planned move in a 2016 interview with then Providence Journal reporter Rich Salit [who now works for Lifespan], in an article entitled, “Hospitals’ goals: Capturing the allegiance of families, so they will be patients for life.”
“For a hospital the size of Rhode Island Hospital, it’s pretty unique that it doesn’t have obstetrics in its portfolio,” Montella said in the story. “Look at adults between the ages of 18 and 44; four out of the five top procedures are related to pregnancy and childbirth.”
The argument advanced by Rhode Island Hospital has also been framed within the concept of an accountable care model as practiced by Lifespan’s Women’s Medicine Collaborative.
“When women receive care in a fully-integrated model like this, outcomes improve, cost-effectiveness and value increase, and women have more choices,” according to Dr. Margaret “Peg” Miller, the current director of the Women’s Medicine Collaborative. [Miller sat next to Bourque at the hearing on May 2.]
Mark Marcatano, president and COO of Care New England, in his testimony before the R.I. Health Services Council on May 2, countered Miller’s argument, saying that “there is no point in developing redundant services” on an ACO delivery model. The more cost effective way of addressing population health management, Marcantano said, was through contractual arrangements rather than through replication of services.
Candid testimony, without having to be polite
The closing testimony at the hearing was given by Patrick Quinn, the executive vice president of SEIU District 1199NE, who offered some frank observations about the two Certificates of Need and the battle over market share by Rhode Island’s two largest health systems.
“I get the luxury of speaking my mind and I don’t have to be polite,” Quinn said, beginning his testimony. “This is wrong time to be duplicating facilities,” citing the ongoing debate about repealing the Affordable Care Act and the huge implications it could have for the state.
Instead, Quinn urged that the ongoing clinical cooperation and collaboration between the two health systems that occurs on an everyday basis be recognized as the best model, rather than trying to make more money off female patients.
Instead of squandering money, Quinn argued, the focus should be on improving patient care.
The reality, Quinn continued, is that when there are fewer patients going through the hospital, when the hospital is doing a better job of taking care of people, keeping them out of the hospital, it can reduce some costs.
But, he explained, it makes it harder to pay for all the costs of the ancillary services that must be there; the unit costs are going to go up. “To duplicate [obstetrics] 400 yards from an existing hospital is really insane,” Quinn said.
In regard to the discussions of what might happen with the proposed merger between Care New England and Partners Healthcare, Quinn said that there would be a number of people who will weigh in on that, including the union.
The merger could happen, it could not happen, there may be conditions attached, Quinn continued. “We should move ahead and renovate the labor and delivery rooms [Women & Infants],” he argued, without waiting to see what happens with the merger.
“We honestly feel that health care dollars should go to the bedside, to maximize the care that patients deserve,” Quinn said, adding that at Women & Infants, there was not a separate Medicaid wing – everyone gets the same care.
Finally, Quinn said that one important advantage that Women & Infants had was the strength of its predominately female workforce. “I raise this issue not be dramatic or shrill,” he said, but there was a real value in having women talk directly to women in triage, when a sexual assault or rape has occurred.