The pursuit of hot air in health care
Business summits on health care are often more revealing about what is not on the agenda rather than what is
In a similar fashion, what would happen in health care workers on the front lines of health care delivery – doctors, nurses, physician assistants, social workers and community health workers – had the opportunity to share their perspective of the current state of affairs? Is it time for them to “act up” and become part of the conversation?
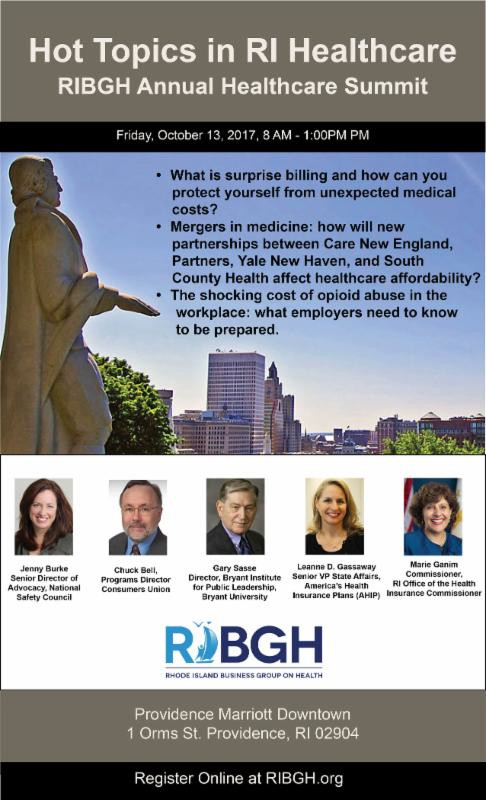
PROVIDENCE – When the Rhode Island Business Group on Health recently sent out a promotional flyer for its annual health care summit, scheduled for Friday, Oct. 13, the teaser under the “hot topics” in Rhode Island health care included: “Mergers in medicine: how will new partnerships between Care New England, Partners, Yale New Haven and South County Health affect health care affordability?”
Whether or not “health care affordability” is the best framework to discuss consolidation of health systems in Rhode Island is open to debate.
A bigger problem with the teaser, no doubt meant to be provocative, is that the statement regarding South County Health and Yale New Haven was misleading and inaccurate, according to Louis Giancola, the president and CEO of South County Health.
When asked by ConvergenceRI to clarify the status of the talks between Yale New Haven and South County Health, Giancola emphasized that discussions were exploratory.
“No, it is still exploratory,” Giancola wrote in an email, explaining that the preliminary talks had not moved to a new level, as had been suggested by the Rhode Island Business Group on Health promotional flyer.
“We have not even signed a non-binding letter of intent. I continue to see it as exploratory,” Giancola continued. “I asked Al Charbonneau [the executive director of the Rhode Island Business Group on Health] to change his flyer as it is very misleading.” [Editor's note: The wording on the flyer has now been corrected in response to Giancola's request.]
Whatever the intent, the apparent inaccuracy of what was happening between South County Health, the only remaining unaligned acute care community hospital in Rhode Island, and its neighbor in Connecticut, Yale New Haven, the current owner of Westerly Hospital, appears to be symptomatic of a larger malady: the rising levels of noise, distortion and avoidance when it comes to discussing the future of health care in Rhode Island, particularly by the business community.
Pay to play
The fees to attend the summit sponsored the Rhode Island Business Group on Health, the statewide trade group of the health insurance industry, are $125 for a non-member, $75 for a non-member guest, and no charge if you are a member.
A week earlier, on Oct. 5, the Providence Business News is scheduled to hold its own annual health care summit, priced at $60 a person or $600 a table.
Translated, like so many things about health care today, the ability to participate in the conversation comes with the requisite co-pay.
At the PBN health summit, there also appears to be a correlation between advertising sponsorships for the summit and those “experts” that have been given a seat at the podium. The overlap includes:
• Peter Marino, president and CEO of Neighborhood Health Plan of Rhode Island; Neighborhood is a partner sponsor
• Dr. Alan Kurose, CEO of Coastal Medical; Coastal is a partner sponsor
• Steve Kozak, director of Behavioral Health Services at Tufts Health Plan; Tufts is a partner sponsor
• Melissa Cummings, senior vice president and chief customer officer at Blue Cross & Blue Shield of Rhode Island; Blue Cross is a presenting sponsor.
What is not on the agenda
There are some similarities in topics to be addressed by both business summits: the costs and impacts of the opioid crisis in the workplace, for instance. Neither summit, however, has invited anyone from the recovery community to share their perspective on how to translate talk into action, particularly around harm reduction strategies.
Imagine, for instance, if PBN and RIBGH followed the lead of the Governor’s Task Force for Overdose Prevention and Intervention, which has challenged the folks planning to attend the Sept. 13 task force meeting to purchase a naloxone kit at a local Rhode Island pharmacy and bring it with them.
How many businesses, for instance, have ready access to naloxone kits in the workplace? Good question.
But there are also more fundamental policy questions that do not seem to be a part of the agenda at either summit. They include:
• The continuing fallout from the botched implementation of UHIP, the more than $400 million Unified Health Infrastructure Project, and the damage it has done to the state’s long-term care infrastructure. Why is this important to talk about? Because efforts by the state to control Medicaid spending under the Reinvention of Medicaid may be jeopardized by the potential loss of federal matching funds, driving the projected budget deficit higher.
• The policy debate swirling around how best to define population health – is it by those enrolled in health plans or is it by zip code – and how that meshes with efforts to address the social disparities of health. Why is this important to talk about? Because future federal reimbursements from Medicaid and Medicare are directly tied to the ability of health systems to manage population health over a continuum of care.
• The legislative efforts to establish a national single payer health system, Medicare for All, to which Sen. Sheldon Whitehouse has just signed on as a co-sponsor in Congress. Why is this important to talk about? Because none of the current Congressional efforts to repeal, replace and repair the Affordable Care Act address the continued escalation of medical costs, which are projected to reach 50 percent of household income by 2025.
• Any discussion of the efforts to establish Neighborhood Health Stations in Rhode Island, which include the current community-based initiatives in Central Falls and Scituate. Why is this important to talk about? The capability of a community-based health center in Central Falls to manage the primary care needs for 90 percent of the city’s residents, coordinated through a sophisticated health IT analytics approach, offers an alternative business model for health care delivery.
• The role of nurses within the evolving health care delivery system in Rhode Island. There are no “nurses” who have been invited to be participants as experts at either of the business summits. Why is this important to talk about? Because nurses hold up more than half the sky when it comes to health care, with increasing responsibilities within a patient-centered model of health care. But, like Rodney Dangerfield, they still “don’t get no respect” when it comes to inclusion in policy discussions, such as business summits on health. This fall, the new joint nursing center, a partnership between nursing programs from URI and RIC, is slated to open.
• The connection between economic disruption and the diseases of despair – the high rate of deaths from alcohol, suicide and drugs. Between 2010 and 2014, according to CDC statistics, Rhode Island led the nation in the number of deaths for white adults between the ages of 25-34 for alcohol, suicide and drugs, which caused 59.8 percent of all deaths for that age group and demographic. Why is this important to talk about? Because without a discussion of the economic disruptions of the middle class in Rhode Island, discussions of behavioral health and mental health interventions do not address the root causes. Also missing from the conversation is the matter of corporate responsibility and liability for the marketing of prescription painkillers.
There are many other important topics missing from the agendas of the two summits: the role of health equity zones, the reasons behind rising pharmacy costs, the role of public health advocacy, the health impacts of climate change, the creation of Brown Physicians, Inc., the translational research enterprise in Rhode Island, the future of the all-payer Care Transformation Collaborative, and the nascent industry cluster of health management firms in Rhode Island.
Finally, there is a sense that the experts recruited to speak at the two business summits on health care represent the usual suspects, a kind of “deadly experiment” of policy talk. Imagine the difference if someone such as Dr. Michael Fine, who is writing a book on the coming health care revolt, were invited to join the conversation and talk about the economics of health care, to make his argument that we do not have a health care delivery system but rather a market to extract wealth? Or, for that matter, if Dr. Peter Simon, retired pediatrician, could talk about public health policy interventions at the community level?
A common denominator
One common denominator for both business health care summits will be the participation of Marie Ganim, the newly appointed R.I. Health Insurance Commissioner.
Ganim replaced Kathleen Hittner in July, who had been appointed by then Gov. Lincoln Chafee in 2013. Hittner had replaced the first commissioner, Christopher Koller.
ConvergenceRI recently interviewed Ganim about how the future role of OHIC in defining the future health care landscape. Here is the ConvergenceRI interview with Ganim.
ConvergenceRI: Is there, as Christy Ferguson said in a recent interview, a move by insurers to develop new self-insured products for the small business group market in Rhode Island? Is there a way to quantify that?
GANIM: We haven’t seen this new product design in our small group market of small businesses with one to 50 employees.
ConvergenceRI: Has Rhode Island seen an increase in the volatility of the individual market?
GANIM: We have been fortunate here; the Affordable Care Act has worked in Rhode Island. We’ve read about 30 percent and 40 percent increases elsewhere. We have not had a crisis in high premiums, compared to other states. We have not seen [that kind of] volatility. We actually saw some decreases in rates.
ConvergenceRI: Will the 2 percent cap on increases paid to hospitals in Rhode Island by commercial health insurers be maintained by OHIC as part of the affordability standards?
GANIM: When Chris Koller [the first R.I. Health Insurance Commissioner] looked at [the differences] in what hospitals were being paid for services, he [looked at] what was the best way to bend that cost curve as part of the package in the affordability standards to ratchet down hospital increases in spending and invest more in primary care [to achieve] the result of better health outcomes.
We are always looking at that package; I can’t say there are not going to be changes. As of January of 2017, new regulations [were put in place] under which [this] particular cap were assessed as the cost of living, using the Consumer Price Index, plus 2 percent.
In 2017, that calculation was an increase to 3.1 percent.
At the same time, the primary care spending by insurers continues to grow. Blue Cross did a story that said for every $1 invested in primary care, there was a $2.50 return on investment.
I think we’re holding firm [on the accountability standards].
ConvergenceRI: How involved is OHIC with the continuing efforts of the all-payer Care Transformation Collaborative?
GANIM: That’s a great question. Commissioner Hittner handed that mantle over to me. The Care Transformation Collaborative has had some remarkable results.
You should talk with Deb Hurwitz, [the co-director of CTC].
So, yes, I’m involved. I am on the board; they look to me for guidance and advice and leadership. I’m part of a leadership team on the board.
ConvergenceRI: What role, if any, will OHIC play in the State Innovation Model [SIM] process moving forward?
GANIM: A very close role. I serve as co-chair of the steering committee. Over the past two years the SIM priorities [have been] aligned with OHIC priorities and been extensions of what this agency is doing, in coordination with the R.I. Department of Health and the R.I. Department of Behavioral Healthcare, Developmental Disabilities and Hospitals.
The staff for SIM – two of them, Marti Rosenberg and Libby Bunzli – are co-located at OHIC. We provide them with data. It is a very close, complementary relationship. We’re very happy [with the progress with SIM].
I haven’t been to a SIM steering committee yet. There is one next week [on Thursday, Sept. 14, where the agenda will include a discussion of patient engagement vendor selection and project overview].
ConvergenceRI: What kinds of data will you be seeking in the future to help guide your decisions moving forward?
GANIM: Once again, a great question. I’d like to take a look at the behavioral health study more closely [the Truven study]. We are looking at market conduct, a deep dive into how mental health coverage is being implemented.
It is an intensive look at records from insurers, to track [the coverage] from the first claim, and see how the insurers [are providing services], to ask if this was the appropriate course of care. The work is being done by out of state consultants, so there are no conflicts of interest.
The study is labor intensive, but at the end, we will have some really good data on behavioral health care and improve that system going forward.
ConvergenceRI: When will the study be completed?
GANIM: We hope to have some preliminary overviews by the end of October. The study involves a detailed legal and regulatory process; a detailed report will be sent to each individual insurer with the opportunity to refute. We hope to have a final report sometime early next year.
ConvergenceRI: In the past, OHIC has been charged by the R.I. General Assembly to be the convener, if that’s the right word, for numerous studies, such as the Truven study. Will OHIC continue to play that role moving forward?
GANIM: I wish I could say. We need resources to do these studies.
ConvergenceRI: How best can consumer voices be heard?
GANIM: I started the week that we held public hearings on rate increases and on Blue Cross Direct Pay. It was my third day on the job.
It was the best way to begin to hear from the public. What the people said is forever ingrained – such as the hairdresser who calculated how many haircuts she had to do to pay for her health insurance
The same week that OHIC approved a rate increase for Blue Cross, a story came out about how Blue Cross reporting a profit for the first quarter, and a woman from Newport County reached out, asking how come the rates went up.
I responded by telling her that Blue Cross had suffered losses over the past three years, and that when we set rates, we set rates looking forward at the margins. That woman thanked us for communicating with her and explaining [the context] of the news article.
That’s the value of communication. I’ve been asked to speak before six groups in the next few months, and I’m going to every one of them [including both the RIBGH and PBN health summits].
We are connected with consumers; they share with us their complaints. We really love that here. It is an important partnership.