Emphasizing the patient in PCMH
As the all-payer Care Transformation Collaborative expands to kids and perhaps to teens, listening to the patients' voices remains a critical need
And, also on Thursday, May 21, the R.I. Senate Committee on Health and Human Services unanimously approved the appointment of Dr. Nicole Alexander-Scott as the new director of the R.I. Department of Health. A full Senate confirmation vote for Alexander-Scott is expected this week; she will succeed Dr. Michael Fine, who resigned in March.
PROVIDENCE – Three years ago, on May 22, 2012, Dr. Patricia Flanagan, a pediatrician, sat near ConvergenceRI at a presentation at the Alpert Medical School at Brown University, listening to a number of national experts talk about the best way to grow patient-centered medical homes, or PCMHs, as a way to transform the business of health care.
The star-studded cast included: Dr. Douglas Eby, vice president of Medical Services for South-Central Foundation, Alaska Native Medical Center; Dr. Craig Jones, director of the Vermont Blueprint for Health, Dr. Paul Grundy, global director of IBM’s Healthcare Transformation; and Dr. Frank Basile, an internist with University Medicine, an early adopter of patient-centered medical homes in Rhode Island,
Right before the session began, Flanagan had wondered out loud to ConvergenceRI: why hadn’t pediatrics been integrated into the PCMH framework? Why had all of the investments gone to identify potential cost reductions in the chronic care of adult population, with little focus on children? Good questions – questions that Flanagan would soon turn around and answer with an action plan.
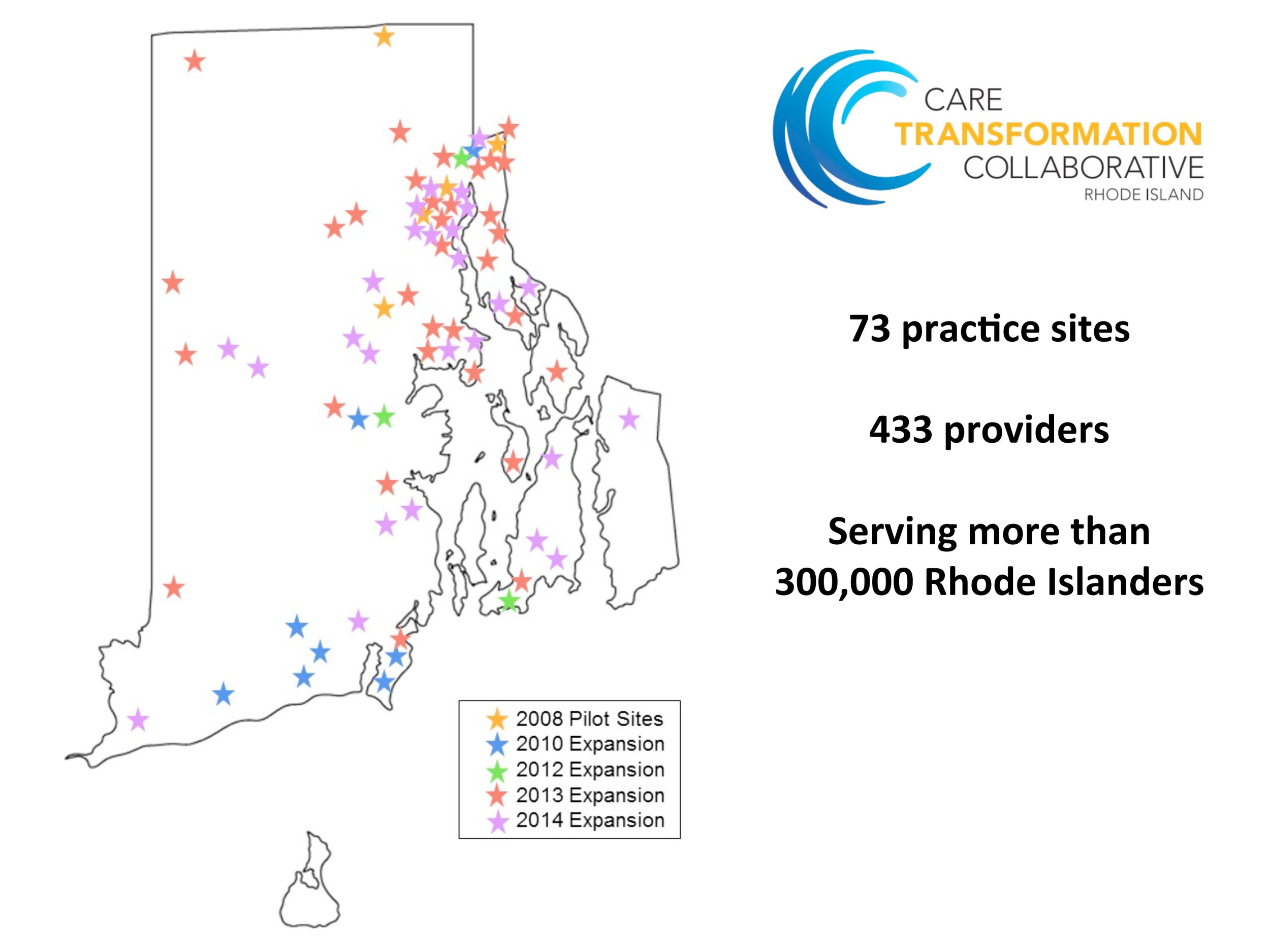
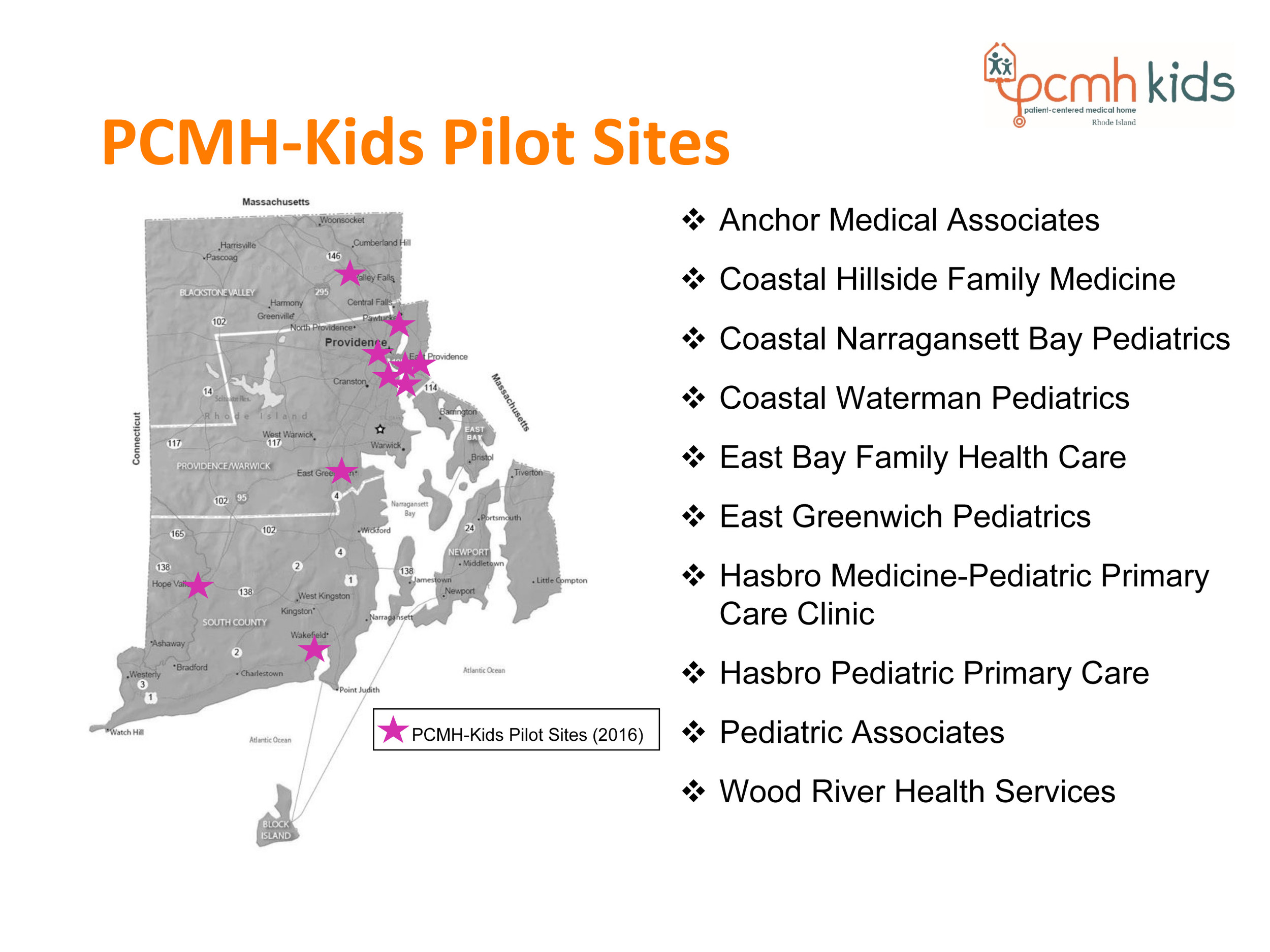
On May 21, 2015, almost exactly three years to the day, Flanagan and her co-chair, Dr. Elizabeth Lange, announced the launch of a new pilot program, PCMH-Kids, as part of the Care Transformation Collaborative [the new name of the R.I. Chronic Care Sustainability Initiative, or CSI-RI], which would include 10 pediatric practices, serving some 30,000 Rhode Island children. The pilot’s first year was funded through a grant from The Rhode Island Foundation, and the initiative was to be coordinated by a team from the R.I. Executive Office of Health and Human Services
Together, with the existing 73 practice sites that serve more than 300,000 Rhode Islanders, the all-payer, patient-centered medical home model now delivers care to about one-third of the state’s population – even if many patients were unaware of that fact.
Listening to the voice of the patient
The event, hosted at the Rhode Island Foundation, featured brief remarks by Neil Steinberg, president and CEO of The Rhode Island Foundation, Debra Hurwitz, co-director of the Care Transformation Collaborative, Dr. Kathleen Hittner, the R.I. Health Insurance Commissioner, Dr. Gus Manocchia, vice president and chief medical officer at Blue Cross & Blue Shield of Rhode Island, Dr. Russ Corcoran from South County Hospital, Dr. Renee Rulin, chief medical officer for UnitedHealthCare’s Rhode Island Medicaid program, Lange, Elizabeth Roberts, secretary of the R.I. Executive Office of Health and Human Services, and Dr. Pano Yeracaris, co-director of the Care Transformation Collaborative.
The messages from this group of health care delivery leaders focused mostly on cost-cutting, alignment of payment models, measuring outcomes, quality, and trends, the integration of behavioral health, the potential of developing a PCMH for adolescents, and the potential to transform the entire health care delivery system in Rhode Island. There was plenty of content to digest; most of the speakers overran their “time is up” notice.
The next big push, many of the speakers agreed, is to move toward a more integrated system of care – one that can integrate behavioral health and expand the scope of the current adult primary care-focused initiative with hospitals, specialists and children.
“Primary care can’t do it alone,” said Hurwitz, talking about the need to transform the way that care was delivered.
But the true star of the morning was Tina Spears, who delivered an emotional story from the patient’s perspective – talking about the importance of being part of a network of care that can listen and respond to the patients’ needs.
Spears began by cutting to the chase – for all the talk of outcomes and statistics, that’s not what patients really cared about, she began. What Spears then told was a personal story of her own experience with her son, born with severe neurological conditions, and how the interactions with her pediatric team – supporting her at the most difficult times – was what primary care should be about.
Spears’ talk – delivered in a halting voice, often punctuated with tears – echoed and reinforced the message that Eby had delivered three years before: the shift is about delivery health in a patient-directed, community context, rather than “disease care.”
It was not just about changing workflow patterns, Eby had insisted, but it began with clinicians “learning to listen at least 10 different ways at all times” – and investment in mentoring for all clinicians and management, as a way to “re-humanize” the story.
“It’s all about the patient’s [and family’s] experience of care,” Spears said on May 21, emphasizing the importance of being heard.
The audience of about 45 warmly applauded Spears; Hurwitz hugged her, and Flanagan gave her encouragement as she took her seat again. Kudos to the Care Transformation Collaborative team for featuring Spears and recognizing that the patient’s voice needs to be heard.
But, apparently, it’s not just the clinicians, insurers and administrators who may need to learn how to listen in 10 different ways. Neither Richard Salit, in his story in The Providence Journal, nor Kristin Gourlay, in her coverage on Rhode Island Public Radio, mentioned Spears – relegating what the patient has to say to the back of the bus in the conversation around health care.
Perhaps, such an emotional, personal story, did not fit well into the easy-to-digest, bite-size news format. As a result, Spears and her very personal story, and her role as the patient advocate, did not exist as part of the reported story in the traditional media.
By leaving Spears out of the coverage, their respective audiences were also excluded and left out of the conversation. [Spears was also left out of the news release.]
Rumblings beneath the surface
In his short, five-minute talk at the event, Manocchia offered up evidence of both the successes and shortcomings of the PCMH initiative – and some hints about new kinds of analytics that Blue Cross is about to launch, related to chronic disease management.
From the good news perspective, Manocchia lauded the progress that the Care Transformation Collaborative had made from an initial pilot program begun in 2008, when it was just “a twinkle in [former R.I. Health Insurance Commissioner] Chris Koller’s eyes,” to its position today in 2015: an all-payer, team-led program with one-third of the state enrolled in PCMH model of primary care, of which there were 72,000 Blue Cross members.
On its own, Blue Cross had invested some $60 million in the PCMH model over the last five years, according to Manocchia.
On the shortcomings side of the equation, Manocchia pointed out that there was a problem of new patients trying to gain access to be seen by PCMH practices, based on calls that he had fielded himself from Blue Cross members.
“New patients can’t get into the practices, because they are not accepting new patients, of if they are, there’s often a six-month waiting period,” Manocchia said.
In turn, Manocchia continued, PCMH practices “will have to move faster,” saying it was more than just accommodating patients’ demand in after-hours convenience.
Mancocchia also seconded the point that R.I. Health Insurance Commissioner Hittner raised in her brief talk preceding him. Hittner said that insurers needed to be able to see the rewards on their investment in primary care through the affordability standards introduced by OHIC.
Manocchia suggested that the next challenge for the Care Transformation Collaborative and its 73 current practices [83 if you include PCMH-Kids] would be how they became integrated in the accountable care organizations and an overall system of care, focused on improvement in care coordination and cost reductions system wide.
Toward that end, Manocchia announced that in June, Blue Cross would be launching a new series of disease registries focused on population health, focused on population health analytics.
[This was big, breaking news; yet it also was not mentioned in the stories by the reporters from The Providence Journal and Rhode Island Public Radio.]
Who’s included in the registry?
Instead of depending on the existing databases at the R.I. Department of Health, or working in collaboration with the state agency, the state’s leading health insurer has plans to develop its own disease database to capture population health management analytics, according to Manocchia.
What did that mean? How would the new disease registries be used? Would the newly announced effort to create a Blue Cross-centric disease registry trigger an “arms race” by competing insurers in the state around data? Would UnitedHealthcare, Tufts and Neighborhood Health Plan of Rhode Island be far behind in mining their own data to create similar, competing disease registries?
When asked, after the event, exactly what those disease registries would be and what diseases they would track, Manocchia declined to share with ConvergenceRI any more details, saying: “Wait until June.” He did agree to forward ConvergenceRI’s questions to Stacy Paterno, the communications director at Blue Cross.
Absent an answer by Manocchia, ConvergenceRI asked others what they thought might be the target diseases – and the value – of these newly announced registries.
[ConvergenceRI also contacted the R.I. Department of Health regarding its existing disease registries, which include a statewide cancer registry and a HIV/STD registry, according to the agency’s website. No response was received in time for the newsletter’s deadline.]
When asked about the value of Blue Cross’s work to develop its own disease registry, one doctor familiar with the state’s health infrastructure and delivery system predicted that the new disease registries would focus on chronic diseases such as diabetes, where the greatest future costs to the insurance system were. The larger question about the value of such a disease registry, the doctor continued, was what part of the population would be captured in the numbers – those insured? Those insured by Blue Cross? Those who are seen on a regular basis by health care providers?
Without the other side of the equation, the uninsured and the under-insured, and those with limited access to care, the numbers in such a disease registry would be incomplete and self-serving, the doctor warned.
Another physician predicted that the disease registry would be targeted toward the Medicare population – particularly the private insurance plans under Medicare Part D, because that was where the money was.
A third physician suggested that one of the targets of the disease registry might be asthma, because that was where the low-hanging fruit would be to reduce hospitalizations and improve adherence to medications, within the context of a patient-centered medical home model.
But, the physician added, without the collaboration around the social determinants of health – such as green and healthy homes – where the potential triggers of asthma were removed, the potential cost-savings realized by the health care delivery system may prove to be not much more than an accounting trick.
PCMH-Kids
The first 10 pediatric practices included in the launch of the PCMH-Kids pilot program include: Anchor Medical Associates; Coastal Hillside Family Medicine; Coastal Narragansett Bay Pediatrics, Coastal Waterman Pediatrics, East Bay Family Health Care, East Greenwich Pediatrics, Hasbro Medicine-Pediatric Primary Care Clinic, Hasbro Pediatric Primary Care, Pediatric Associates, and Wood River Health Services.
The program had been developed in consultation with a 35-member stakeholder committee, according to Lange, with the mission to extend the ongoing transformation of primary care to pediatrics, focused on “multi-payer payment reform and data-driven quality improvement.”
The key goals for the pilot program’s first year are focused on defining common ground for the practices: to negotiate a common contract; to define care coordination roles and responsibilities; to integrate PCMH-Kids into the broader existing structure of the Care Transformation Collaborative; and to develop a “tier per member per month” payment system based upon medical complexity.
The tiered payment system, not defined in the documents, apparently speaks to the kinds of patient-care required in complex cases for children, an issue that cuts across many concerns around cost and management of care.
As one pediatrician told ConvergenceRI a few days after the event, there was a need to define what integration meant in bringing together the existing scope of services in a comprehensive fashion. Kids who are being screened for developmental and behavioral delays, the physician continued, may need access to services that are not always seen as medically necessary by health insurers, such as early intervention, full-day preschool with a focus on executive functions, emotional competency and language acquisition. How will PCMH-Kids track how practices provide behavioral and developmental interventions for children who are being screened at 30 months?
Somewhat surprisingly, none of the larger community health centers that serve the largest number of children in Rhode Island’s urban centers are participating in the pilot program – in Woonsocket, in Pawtucket and Central Falls, or in Providence. That may change as the program expands beyond its pilot status.
The lack of participation is rumored to be about disagreements about financial support in terms of rates of reimbursement offered by Neighborhood Health Plan of Rhode Island, as directed by Rhode Island’s Medicaid office under R.I. EOHHS.
Two separate conversations about health care – and health
Most of the speakers at the event talked about the need for health care delivery transformation: the need for alignment with the change in business models from fee-for-service to accountable care organizations around a continuum of care; the potential of the $20 million State Innovation Model grant to provide impetus for that transformation; and the goal of having 80 percent of Rhode Island’s population receiving primary care through a patient-centered medical home model.
Still, there are two distinct rivers of conversation in Rhode Island that often come close but don’t ever seem to intersect or converge with care transformation: the effort now underway to develop 11 health equity zones as a community-based investment in health, wellness and prevention; and the effort to develop an alternative model of the neighborhood health station, the first such enterprise now underway in Central Falls and Pawtucket. [See link below to ConvergenceRI stories.]
There is clearly a need to map health innovation in Rhode Island – not just as a factor of health care delivery transformation, but fully integrating the social determinants of health from a community and patient perspective.
The work being done to develop a working definition of toxic stress for purposes of diagnosis, treatment and referral within the world of pediatrics, combined with the home visitation programs being coordinated by the R.I. Department of Health, and integrated with the work underway through the R.I. Alliance for Green and Healthy Homes, and the evidence-based research focused on early childhood interventions and outcomes, offer a compelling case for convergence.
The richness of Rhode Island in being a small place that can develop a nimble, coordinated response in the world of health innovation needs to become part of Rhode Island’s competitive advantage.